Using Analytics For Healthier Encounters
By Oleg Issers, X by 2

It’s no secret that a new business model has been emerging for the healthcare industry over the last several years. From its early days at the end of the previous century, the Managed Care model has slowly but surely been making its way into every nook and cranny of an industry desperately in need of reinventing itself. The reasons for this are many, but at its core, the promise of a healthcare delivery system organized to manage cost, utilization and the quality of healthcare services is just too promising to ignore.
The Managed Care process has also introduced a very powerful concept to the industry: that of shared risk and shared rewards between healthcare providers and healthcare insurers. But while conceptually compelling, the actual implementation of the model in the real world of day-to-day healthcare in this country has proved daunting to say the least.
One of the key success factors for the successful implementation of the Managed Care model – and specifically for the shared risk and rewards approach – is the utilization of high-quality data and the analytics it can produce. Without the data to accurately verify patient, provider and payer performance the whole model becomes sub-optimized. To make sure that the data does, in fact, tell a comprehensive story, many providers and insurers are focusing on improving their claims analytics data, and particularly the idea of a Healthcare Encounter.
Simply put, a Healthcare Encounter is an interaction between a person (patient) and a healthcare provider. In the context of claims analytics as an example, providers are categorized as a professional (an individual medical practitioner) or a facility (a hospital, outpatient clinic, laboratory, etc.). Further, professional and facility providers submit different types of claims to payers (health insurance companies) for reimbursement. In the context of claims then, a Healthcare Encounter can be defined as a grouping of related claims for the same person, provider, payer and date range.
An example set of business rules for a Healthcare Encounter can help illustrate this approach:
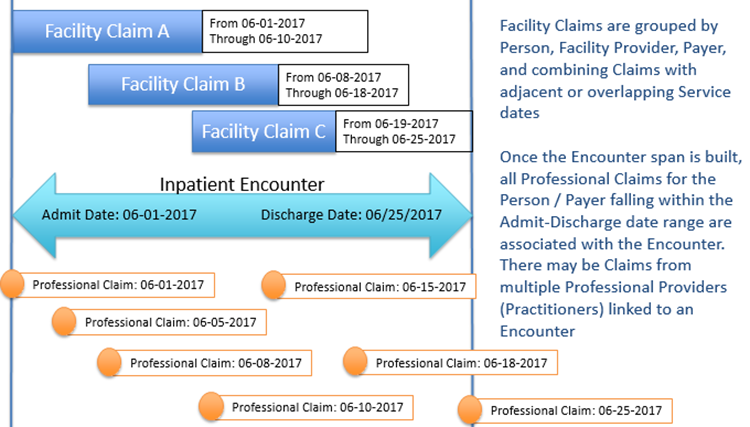
Illustration: Grouping of Facility and Professional Claims to build an Inpatient Encounter
Facility Inpatient Encounters
These typically span multiple days. Encounter date range is built by grouping related Facility Claims (same Person, Facility Provider, Payer, Diagnosis, and adjacent or overlapping date ranges). Any Professional Claims for the same Person within the date range are linked to the Inpatient Encounter; there may be claims from multiple Professional Providers (Practitioners) linked to the same Facility Encounter.
- Skilled Nursing Facility or Nursing Home Encounter
- Hospice Encounter
- Home Health Encounter
- Acute Inpatient Hospital Encounter
- Inpatient Mental Health Encounter
- Inpatient Rehabilitation Encounter
Facility Person-Day Encounter
These follow the same business logic as Facility Inpatient but only span a single day – no merging of Claims with adjacent dates. An assumption is made that any Professional medical services the Person received on the same day are related to the Person-Day encounter.
- Observation Encounter
- Emergency Room Encounter
- Urgent Care Encounter
- Outpatient Surgery Encounter
Facility Outpatient Encounter
Facility Claims are grouped by Person, Facility Provider, Payer and Service Date. No merging of dates or linkage of Professional Claims.
- Dialysis
- Physical Therapy
- Occupational Therapy
- Radiology
- Lab/Pathology
Professional/Ambulatory Encounter Types
Professional Claims are grouped by Person, Professional Provider (Practitioner), Payer and Service Date.
- Administered Drugs, including Chemo Drugs
- Allergy Encounter
- Cardiovascular Encounter
- Surgery Professional Encounter
- Among others
The concept of a Healthcare Encounter is a powerful one. It starts to address the issue that many large providers encounter when accepting patient healthcare insurance from a multitude of insurers. The providers need a more efficient way to identify multiple insurance payers for the same patient.
One way to think about the concept of Healthcare Encounters is to imagine a “day-in-the-life” of a patient who has multiple outpatient appointments that might include a consultation, a procedure, blood work, physical therapy, etc., all from potentially different facilities and payers. The concept of the Healthcare Encounter pulls all these disparate encounters together into a more meaningful way to manage healthcare claims. Additionally, this concept goes right to the heart of the Managed Care model’s requirement for the kinds of analytics that can truly produce the quality risk measures needed to accurately and effectively assess provider performance.
There are, however, still obstacles to achieving the promise of the Healthcare Encounter concept. First and foremost, overall industry cooperation when it comes to data and analytics needs to improve. As of now, there is not a common and accepted set of data quality standards across the healthcare industry. Such standards are a critical part of the ability to create the kinds of advanced analytics required to support the dreams of the Managed Care model – inclusive of the Healthcare Encounter concept - in the industry. While progress has been made on optimizing and standardizing data code sets in the industry, there is still much work to be done.
The healthcare industry is fast approaching a critical inflection point. There is wide consensus that the Managed Care model remains the future of the industry, leading to better overall health, service, and satisfaction for patients, and better overall process, efficiency, and profitability for providers and insurers. The key to really achieving all of that is data analytics for verification and continual improvement. In this area, much work needs to be done.
