The Patient Experience Is Clinical

By Mark Crockett, CEO, Verge Health
As quickly as healthcare began to focus on patient experience, the law of unintended consequences kicked in. While well received as a tool to help improve care, this situation unintentionally gave rise to a consumer culture around patient treatment. Today’s value-based care arrangements call for providers to take a fresh look at patient experience.
While patients certainly deserve to be treated with dignity and listened to carefully, the top patient experience expectation is receiving safe, quality care. “Patient experience [is] not about making patients happy over quality,” says Dr. James Merlino of the Association for Patient Experience. “It’s about safe care first, high quality care, and then satisfaction.”
The best way to deliver on this expectation is for providers to view these issues of safety, risk, and compliance as a cohesive whole, thus enabling patients to receive the safe, quality care they expect in the caring and supportive environment they deserve.
Defining Patient Experience
The Beryl Group defines patient experience as “the sum of all interactions, shaped by an organization’s culture, that influences patient perceptions across the continuum of care.” That’s a big job. Most providers lack the tools to make that happen. Where to start? It begins with developing provider/patient and provider/organization relationships that encourage collaboration.
In 2013, a British Medical Journal review of 55 studies found patient experience is “positively associated with clinical effectiveness and patient safety, and supports the case for the inclusion of patient experience as one of the central pillars of quality in healthcare. Clinicians should resist sidelining patient experience as too subjective or mood-oriented, divorced from the ‘real’ clinical work of measuring safety and effectiveness.”
What the BMJ study revealed, and my own anecdotal evidence bears out, is if a patient experience is positive, the patient feels empowered and can enter into a therapeutic alliance with the provider. Patients are motivated to follow treatment plans, and less likely to withhold information, if they don’t feel intimidated — or worse, ignored — by their provider and the hospital where treatment was rendered. This supports swifter diagnoses and improved clinical decision-making and leads to fewer unnecessary referrals or diagnostic tests.
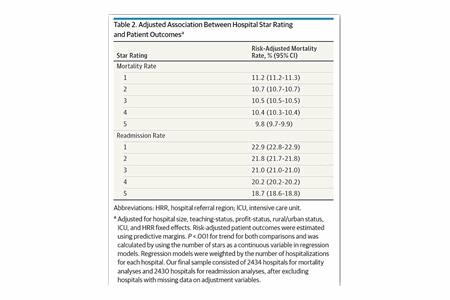
Many hospital CFOs don’t need the BMJ study to know a positive patient experience is a clinical indicator that ties to financial outcomes. As outlined in Figure 1 below, patient experience is directly associated with a hospital’s Star Rating and patient outcomes:
Patient Expectations: Keep Me Safe, Heal Me, And Be Kind To Me
Creating a positive patient experience, and better clinical outcomes, begins with an understanding of what patients expect from providers. The primary expectation of any patient is, first and foremost, safety. To the unfamiliar, hospitals are scary places. Patients no doubt have read or heard stories (or watched doctor shows on TV) of medical errors and medication mix-ups or of being treated by an unqualified caregiver. Hospitals and other healthcare settings must communicate clearly theirs is a safe place where patients can trust their caregivers.
If patients believe they are in a safe, trusted environment, their next expectation is, of course, to get better. To be healed. This requires consistent excellence across a wide variety of performance areas. Finally, patients expect to be treated with courtesy and respect.
Creating The Patient-Centered Culture
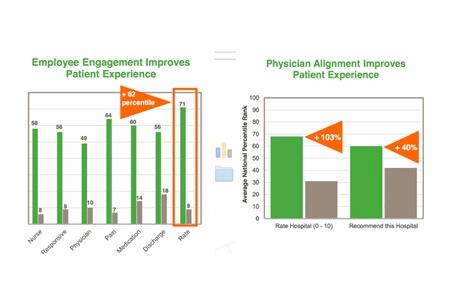
How do we establish patient experience as one of the pillars of quality healthcare? Not surprisingly, it’s a judicious combination of technology, effective communication, and employee engagement and physician alignment.
- Technology
Most patients assume all clinicians are highly qualified and fully credentialed. A robust credentialing platform helps providers deliver on that assumption. Another example of technology impacting patient experience - Communication
Effective communication improves not just patient satisfaction, but also physician satisfaction. It boosts patient adherence and compliance and reduces medical errors and malpractice claims. The benefits of a culture that encourages open, honest, and direct communication among patients, providers, and staff go directly to the heart of patient experience. - Employee Engagement
There is a tremendous benefit to incorporating digital rounding (levering mobile technology to gather information in real-time during the rounding process) into a health system’s employee engagement strategy to generate information from patient rounding, safety rounding, and leader rounding. There is much to be learned from the voices of providers, patients, and employees. For example, although nurses and physicians generate an equal number of complaints, nurses are three times more likely to have positive reports as compared to MDs. However, physician complaints have higher severity and fewer resolutions.
Patient feedback gathered through a rounding process identifies critical focus areas including peer review events, compliance events (particularly in infection control), and patient and employee safety issues.
For one healthcare system, more than 50 percent of all peer review cases at its 30 facilities actually began in patient relations. In addition, validation audits from compliance organizations (specifically CMS) often stem from a patient complaint. Another reason to centralize data gathered from the feedback of patients, providers, and employees is to identify patterns that allow organizations to transform risk management from a reactive process to a proactive component of healthcare delivery.
Patient experience is clinical. It matters to value-based care and has direct impact on an institution’s long-term financial survival. Organizations that sideline patient experience, or simply meet the minimum standards required, do so at their peril.
About The Author
Mark Crockett, MD, FACEP, is the Chief Executive Officer of Verge Health. He will expand on the points raised this article in a presentation, Patient Experience in High Reliability Organizations, at the HIMSS Annual Conference & Exhibition in Orlando, FL.
