5 Steps To QPP Compliance

By Timothy Mills, Chief Growth Officer, Alpha II
Physician practices ignore the new Medicare Quality Payment Program (QPP) at the risk of their financial future. While not participating is an option, that choice will lower your practice’s Medicare reimbursement rate by 4 percent starting in 2019 — so it’s really not an option to consider.
The following five tips will help you understand QPP, why it’s important to participate, and steps your practice should be taking now.
- Arm Yourself With The Correct Information
The Quality Payment Program continues the march from fee-for-service to fee-for-value, rewarding high-value, patient-centered care. The QPP was authorized through the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), which replaces the much-despised Sustainable Growth Rate formula. Collection of reporting data began on Jan. 1, 2017, but physicians and practices still have time to set up a program that will reap substantial benefits in subsequent years.
- Decide What Path Your Practice Will Take
QPP has two pathways, although most physicians are expected to take the first approach.
- Merit-based Incentive Payment System (MIPS), where participants can earn reimbursement bonuses based on quality and reporting metrics.
- Advanced Alternative Payment Models (APMs), a more ambitious innovative payment model.
You are eligible to participate in MIPS if you bill more than $30,000 to Medicare and provide care to more than 100 Medicare patients per year. The program is open to:
- Physicians
- Physician Assistants
- Nurse Practitioners
- Clinical Nurse Specialists
- Certified Nurse Anesthetists
- Educate Executives And Others Who Will Be Involved
The MIPS data aggregation is designed around the four categories of clinical care shown below. Providers will receive a composite score based on performance across all the categories, where the weight for each category varies.
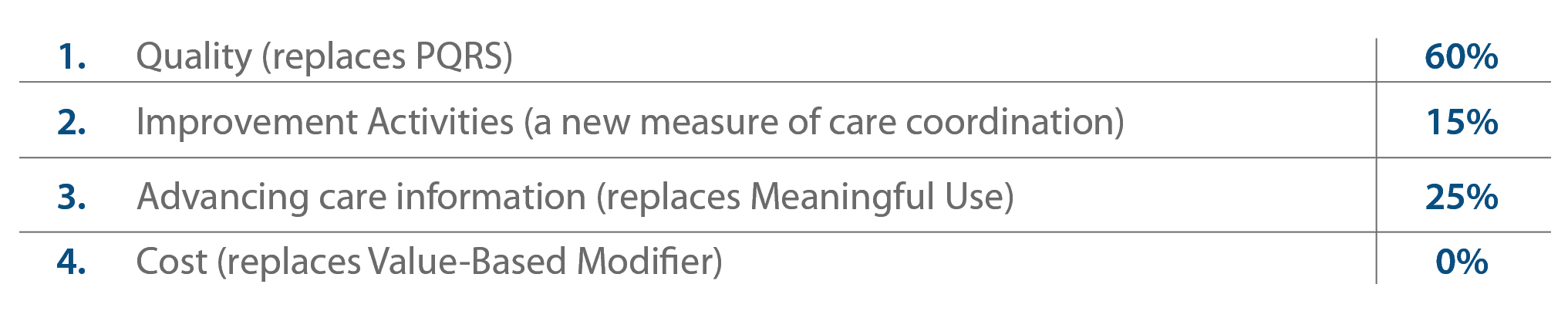
As you can see, quality measures comprise 60 percent of the score and advancing care information accounts for another 25 percent, making a substantial increase in reimbursement possible with little effort. Tracking just one quality measure is enough to negate a reduction in the reimbursement rate in 2019.
It’s important you educate appropriate stakeholders and those who will be responsible for implementing and monitoring this important program. Managing this change process for your team can be the most difficult part. Rather than presenting this as a “stick” the practice must endure to avoid a reimbursement reduction, try presenting this as a “carrot” to provide higher quality care and outcomes to your patients.
- Be As Aggressive As Possible
At the least, the Affordable Care Act faces a myriad of changes under the new administration. But the push toward value-based care shows no signs of slowing down. Industry leaders have recognized fee-for-service alone is no longer the delivery method of choice.
Rather than wait for the changes to engulf your practice, we recommend looking at QPP and MIPS as opportunities to explore new ways to deliver better care. Higher reimbursements are available for practices that track a minimum of six quality measures, track one outcome measure and participate in at least one project designed to improve care coordination. Practices that don’t go at least this far risk leaving reimbursement funds on the table.
- Know When You Need Help
Pulling quality measures from claims data and coding correctly in the first place can be a painstaking processes, so you need to evaluate the competencies of your staff and the structure of your organization. Although participating in MIPS will be a team effort that requires energies from several stakeholders, one person should be in charge of the project. This set-up will help preserve accountability.
While some activities of MIPS likely can be managed internally, other portions you may consider outsourcing to a competent partner. When evaluating potential partners, look for companies that work across the care spectrum, with physicians, practices, clearinghouses and practice management/EMR vendors. A partner should work with companies like yours and offer best practices that you can apply to your practice.
When submitting data to CMS, it’s advisable to use a qualified registry. Your partner should be able to handle the reporting aspect, too.
