Reimagining The Future Of Hospital Crisis Management
By Terry Zysk, LiveProcess

COVID is the trigger that may be the ultimate transformation in healthcare. When the pandemic first hit, health systems went from managing a crisis occasionally to managing multifaceted situations every day. Healthcare organizations needed to reinvent themselves quickly and implement new approaches to everything. This ranged from workforce protection, supply chain and resource stabilization, patient flow and care protocols, and staff communication and engagement – all while dealing with a deadly respiratory pandemic, financial uncertainty, and typical seasonal emergencies, such as tornadoes.
With new challenges come new opportunities, such as how health systems can reimagine themselves to have more effective communication, collaboration, and decision making while at the same time staying financially sound. Here, we’ll take a deeper look at what a reimagined hospital crisis management model could look like soon.
What’s The Current State Of Hospitals And Healthcare Systems?
Since the pandemic, many healthcare organizations are experiencing dramatic fluctuations in patients. As expected, there are ebbs and surges of COVID-19 patients. But there have been other business impacts as well, such as addressing the backlog of delayed elective and non-urgent procedures, and the patients’ reluctance to visit the ER with non-COVID-19 concerns. This pandemic has highlighted that health systems need to be better prepared to innovate and rapidly adapt to thrive.
What Technology Needs To Be In Place To Support The Hospitals Of The Future?
The reality for too many healthcare systems is that real-time situation awareness doesn’t exist. Departmental systems cannot communicate with each other effectively, leading to delays in reporting, delays in decision making, and delays in patient care. Hospitals need real-time health systems (RTHS) to provide situational awareness and close collaboration across clinical, operational, and business domains.
"An RTHS will acquire and correlate situational awareness data and operational intelligence in real-time and apply that insight to ever-changing circumstances surrounding the patient to improve care and operations," said Barry Runyon in the Gartner “Healthcare Provider CIOs: Overcome COVID-19 Challenges With Real-Time Health System Technology.
RTHS will provide better situational awareness, the ability to maintain an understanding of what’s going on around you at every moment and using that information to mitigate risk. This helps healthcare providers and hospitals improve patient outcomes.
The hospital of the future will take real-time situation management to the next level. For example, Riverside County Emergency Management Healthcare Coalition is ahead of the curve and serves as a role model for what is possible in healthcare.
During the pandemic, Riverside was able to embrace real-time situational awareness and swiftly respond to a variety of changing situations. Riverside did this by standardizing on a real-time virtual situation and emergency management platform.
The shared platform provides situational awareness to California county’s 17 acute-care hospitals, 54 skilled nursing homes, and more than 300 clinics, urgent care centers, tribal health clinics, and other facilities. It regularly partners with local governments, school districts, utilities, city planners, military, police, fire departments, and the FBI.
By uniting clinical, operational, and environmental staff into a virtual situation center, Riverside has been able to connect, coordinate and collaborate across departmental, organizational, and geographic boundaries — consistently and in real-time for proactive situation management.
What Is The Difference Between A Physical And Virtual Command Center And Which Is Better?
A hospital command center is the “hub” that manages all patient throughput activities—inbound, within, and outbound. Most hospital command centers are physical buildings that are staffed 24/7 by professionals who can make rapid, effective decisions around patient care. Command centers utilize advanced predictive analytic technology and artificial intelligence to monitor and target real-time data on incoming patients, patient discharges, bed availability, and other hospital logistics.
However, there are limitations to a physical command center. First, everyone needs to physically be in the command center to know what is going on instead of potentially being more helpful in the field. In addition, information sharing generally occurs by word of mouth or requires dedicated transcriptionists to transcribe and disseminate information to those that aren’t in the command center which delays the process and ultimately patient care.
A virtual command center or situation room provides an alternative to 24/7 incident command center staffing. It still requires staffing 24/7 in 12-hour shifts, but command center staff don’t need to be in the same physical location to manage an event. Through a secure web-based application, staff can share information and manage patient surge events from any location with multiway communication and collaboration. Built-in virtual situation rooms work across boundaries to enable all providers and enablers of care to act in unison to ensure the best possible outcomes during routine, urgent, and emergency scenarios.
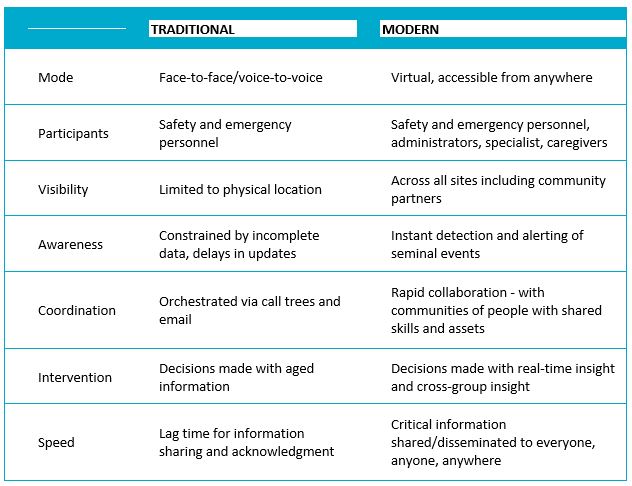
Comparison Of Physical Vs Virtual Command Centers
Where Do We Go From Here?
The health system landscape has significantly changed the past 6 months. Hospitals went from preparing for seasonal flu outbreaks, and occasional blizzards and hurricanes to managing a global infectious disease pandemic. This large-scale unparalleled event has had an enormous impact and put a strain on our hospital resources and supplies in ways that most of us have no experience dealing with daily. This type of situation may last for months and may recur. If this is the new normal, how do we prepare for and transition to this kind of operating model?
The key lies in acting in unison which means the comprehensive coordinated orchestration of all healthcare providers, all devices, all locations, and all organizations. Today, clinical, environmental, and operational domains mostly operate in isolation from one another. Yet, the hospital of the future will work at the intersection of these domains enabling real-time situation management.

By connecting these domains, hospitals of the future will have unified communications at scale and experience interactions they never considered possible. When everyone is connected, common insights can be leveraged across the organization allowing all healthcare providers to respond in unison, without delay and ultimately make the best decisions possible for their patients.
About The Author
 Terry Zysk joins LiveProcess as Chief Executive Officer with more than 20 years of executive leadership. Before LiveProcess, Terry was the Senior Vice President of Operations at MedVentive where she was retained by the CEO to prepare the organization for operational excellence in the rapidly growing market sector, Population Health. Under Terry’s guidance, time to revenue accelerated by 15 percent and the customer base grew 3-fold. She saw MedVentive through the successful acquisition by McKesson in 2012 and remained with McKesson through the transition.
Terry Zysk joins LiveProcess as Chief Executive Officer with more than 20 years of executive leadership. Before LiveProcess, Terry was the Senior Vice President of Operations at MedVentive where she was retained by the CEO to prepare the organization for operational excellence in the rapidly growing market sector, Population Health. Under Terry’s guidance, time to revenue accelerated by 15 percent and the customer base grew 3-fold. She saw MedVentive through the successful acquisition by McKesson in 2012 and remained with McKesson through the transition.
