Participation Powers Healthy Changes: Proven Group-Based Intervention
By Felipe Lobelo, MD PhD, FAHA, Phil Trotter, B.S., Ashley John Heather, B.A., and F. Peter Brechter, B.A.

Health systems urgently need to manage chronic diseases as 86 percent of each U.S healthcare dollar goes to chronic disease related care. Astoundingly, chronic diseases are the leading cause of death and disability worldwide. New York based Off The Scale Health has combined the best technology with the best of group-based intervention to address the epidemic in a new and novel way.
ABSTRACT:
The obesity epidemic (36 percent of adults age 20 an over in the US according to the Centers for Disease Prevention and Control, 2014) has prompted the development of clinical and non-clinical solutions. The real threat of obesity is the impact and expense associated with multiple chronic diseases that are related to obesity as a key risk factor. This white paper focuses on a novel yet practical solution which has been developed by New York based Off The Scale Health. The company’s solution is the Behavior Change Intervention or ‘BCI’.
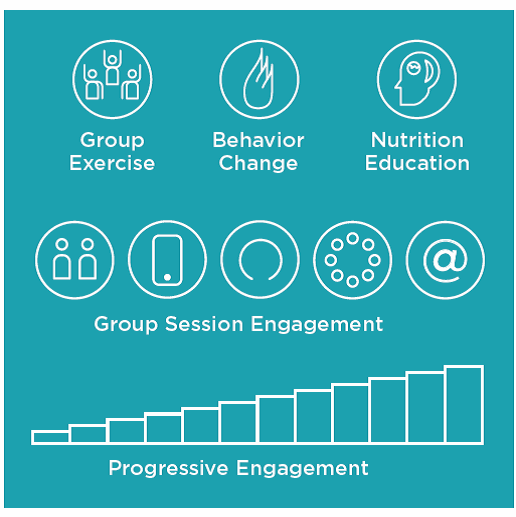
The novel approach of BCI is its marriage of state-of-the-art 24/7 digital tracking, analysis, and communication technology with proven face-to-face peer group lifestyle modifications, applicable nutritional information, and support of self-management. Unlike digital and in-person only chronic disease prevention programs, BCI is focused on patients who have one or more diagnosed chronic diseases. By marrying the best of digital and in-person engagement experiences, BCI elevates levels of participation and condition self-management to slow, stop or even reverse the progression of chronic diseases.
Early indications show that the Off The Scale BCI has considerable real world successes:
- 76 percent lost weight during the initial 12 week intervention
- 82 percent reduced their body fat index during the first 12 weeks
- Participants increased physical activity 12 percent over the initial 12 weeks
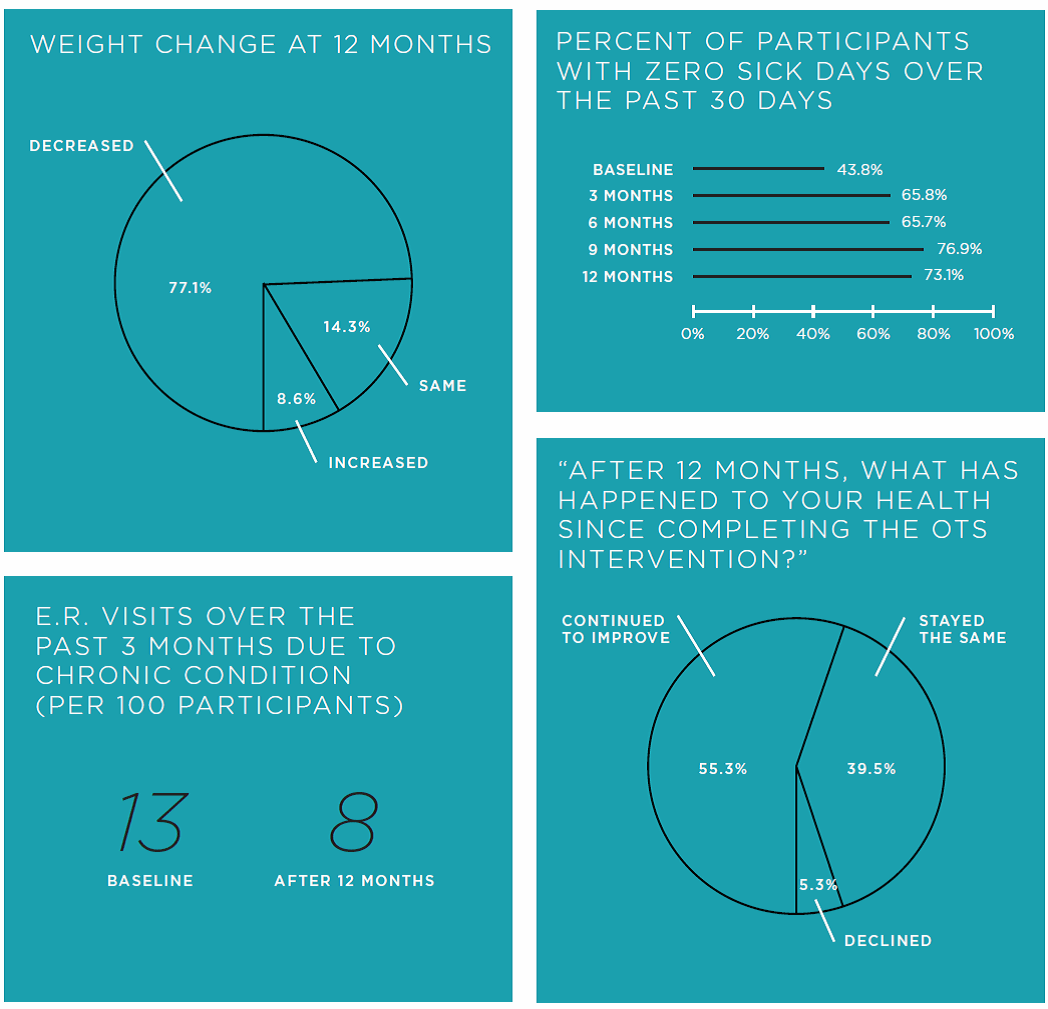
Long term results were strong at 12 months:
- 77.1 percent continued to lose weight week 12 to month 12
- 14.3 percent maintained their weight week 12 to month 12
- 8.6 percent gained weight week 12 to month 12
Fixing Chronic Conditions Before They Become Acute
In the U.S. alone, over 100 million adults are living with prediabetes or diabetes, and more than half of American adults have been diagnosed with one or more chronic conditions. Chronic diseases are the number one threat to American health.1 The evolution of non-medical chronic disease management strategies is taking place as health systems begin to intervene before a patient’s chronic condition reaches the clinical care stage. Many systems are now focusing specifically on intervening in rising-risk population groups with one or more chronic diseases. These systems aim to fill a key care gap by supporting chronic condition self-management programs to tackle the root causes of unhealthy behaviors. This is where participation in behavior change interventions becomes a strategic priority.
Value-Based Care Introduces PHM
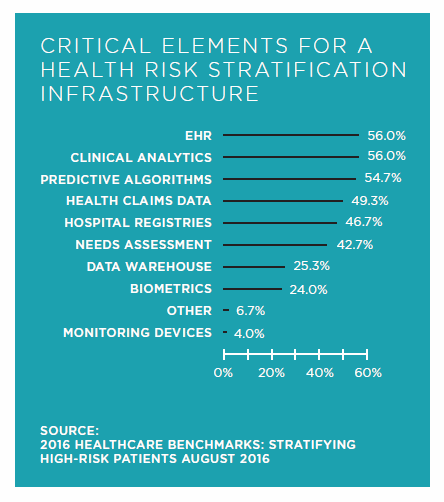
U.S. healthcare is slowly transitioning from volume-based “sick” care to a more proactive, value-based “health” care. Health systems are adopting population health management (PHM) strategies to advance their transformation to value-based care by identifying chronic disease population groups. Leading health systems have PHM stratification analytics to identify health risks based on clinical, claims, and other data sources. With this data, health systems can identify those patient population groups that require chronic disease intervention care.2
Chart 1: Critical Element for a Health Risk Stratification Infrastructure
Lifestyle Behavior Change Effectiveness
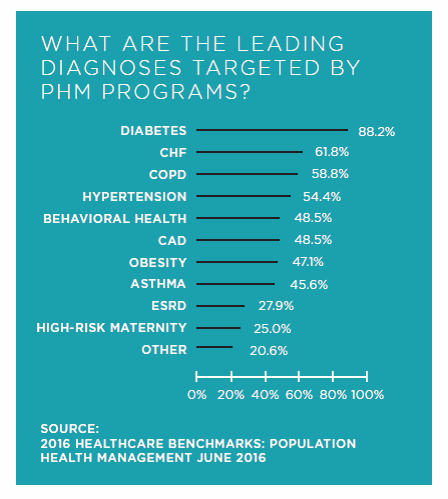
Behavior change programs can be applied to support a variety of diagnosed chronic illnesses and targeted population groups. Intensive lifestyle modification programs are designed as an effective behavior change approach made up of multiple engagement components. These programs include the delivery of processes and group session peer support to facilitate the behavior change of unhealthy keystone habits, practice skills for problem solving, and advance self-management of their chronic conditions.
For patients diagnosed with one or more chronic conditions, there is strong evidence that chronic disease intervention and management programs improve quality of life and health outcomes while reducing healthcare costs. Different populations may need modified behavior change interventions that will work better depending on the community, neighborhood, city, or state of deployment. Therefore, population health demands specific stratification scoring and impactability scoring to risk adjust both program processes and expected outcomes.
Proven program elements can only be useful with high levels of participation to achieve self-management. It is therefore important for clinical care teams and community care teams to collaborate on care plans with participants to identify obstacles, set priorities, and establish goals for participation.
PHM stratification is helping health systems to identify chronic disease population groups and anticipate trends. It also helps pinpoint the gaps in delivering care to these groups.
Chart 2: What Are the Leading Diagnoses Targeted by PHM Programs?
Self-Management As A Cornerstone
Payers and providers acknowledge self-management is the cornerstone goal for chronic disease management, and behavior change intervention is the tool to achieve it. Health systems typically do not have the workforce, the training, or the time for meaningful patient engagement to deliver intensive lifestyle interventions. However, providers do have care coordinators who can navigate rising risk population groups from clinical care into community care where behavior change programs are an effective solution. In the community environment these programs can also take place in localities and at the times that are convenient for the patients and less expensive for the payer.
To balance outcomes with affordability, delivery of behavior change programs must move beyond the four walls of clinical care, and take advantage of lower cost community settings. Thanks to healthcare payers now reimbursing for the delivery of lifestyle modification programs, the evolving non-medical payment landscape offers a unique opportunity to expand efforts around the delivery of behavior change interventions. Payers and providers financially vested in risk-arranged population health contracts are most likely to benefit from their groups participating in behavior change programs that will help slow, stop, or even reverse the progression of chronic diseases.
Behavior Change Program Implementation
The Mount Sinai Health System (MSHS) is pioneering a non-medical outpatient program that targets rising-risk chronic disease population groups. The program is called Off The Scale (“OTS”) and the curriculum is called the OTS Behavior Change Intervention (or “BCI”). The OTS BCI is a hybrid delivery methodology combining high-touch in-person group meetings with sophisticated digital engagement tools and deep social support. This OTS intensive behavior change program is currently being delivered to select Mount Sinai employees exhibiting markers for two or more lifestyle-based chronic diseases, and will eventually be offered to value-based care contracted payer populations. To strengthen their PHM strategies for chronic disease management, MSHS deployed OTS at their facilities for employees to conveniently attend onsite sessions.
Intensive lifestyle interventions do not always have evaluation processes in place to monitor what cohorts are doing and what results are being achieved. In contrast, OTS has defined specific metrics with MSHS and made them a part of their partnership goals. OTS captures data digitally from participants and facilitators to analyze baseline data and adjust in-person session curriculum. OTS’ digital platform tracks a multitude of personal movement, diet, and sleep activities in addition to group attendance, planned digital contact points, use of the digital support tools, participant satisfaction, and connections with other community resources. Most importantly, the OTS BCI surrounds the participant with multiple touch points to drive participation.
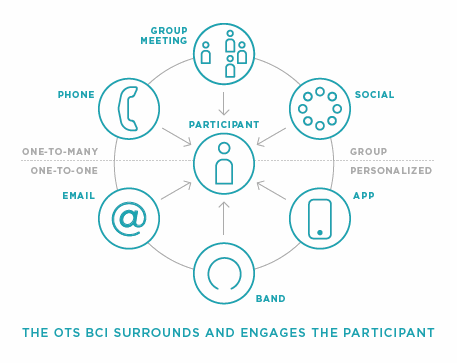
Diagram 1: Cohort Behavior Change to Self-Manage Chronic Diseases
There is strong evidence that the OTS delivers chronic disease self-management, improved quality of life, and positive health outcomes for chronic disease cohort participants. OTS starts with an intervention model that is replicated consistently for structure, processes, and outcomes.
Diagram 2: OTS Behavior Change Intervention (BCI) Model
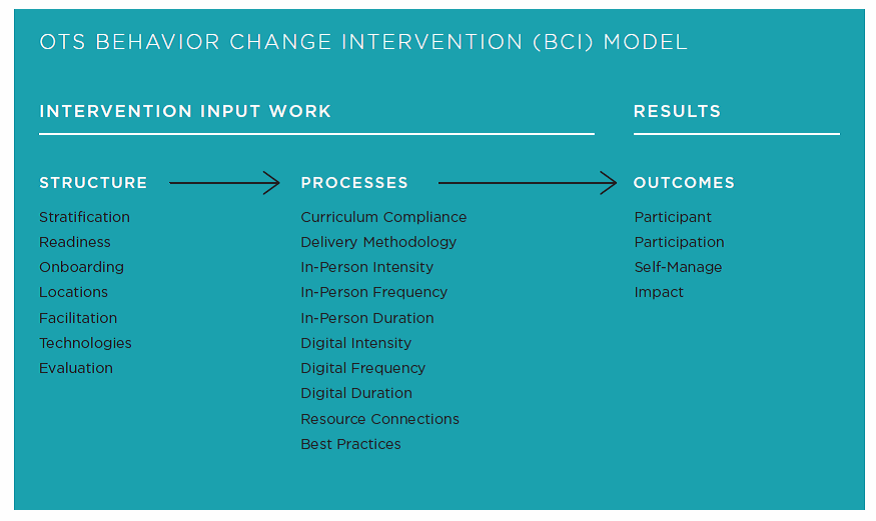
The OTS Behavior Change Intervention (“BCI”) structure collectively optimizes engagement of stratified population groups by analyzing readiness assessment and following onboarding procedures to assemble cohorts at a selected convenient location. The core sessions are then adjusted to fit the profile of the cohort assembled to maximize the opportunity to change their behavior and achieve self-management. OTS tracks process indicators for the cohorts, and analyzes participant evaluations that provide evidence of intervention effectiveness. In doing this OTS has established standards of success that health systems and payers can measure from the core sessions, maintenance program and sustainability support system. This monitoring can be shared with the payers and providers responsible for a population group.
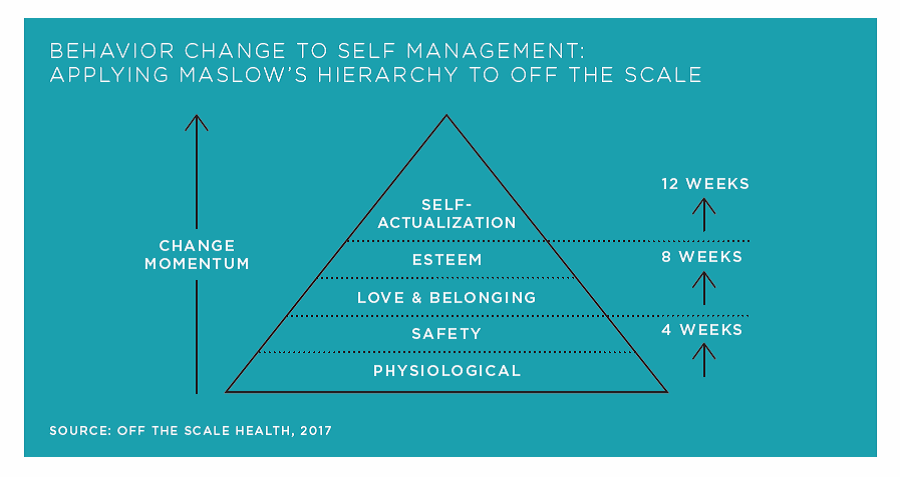
OTS’ success is due to progressive intensity, frequency, and duration of the in-person and digital engagement during the core intervention. This is delivered in a consistent manner across all classes by OTS coaches to slow, stop, or even reverse the progression of cohort disease states. OTS sees its goal as building a “firewall” against chronic diseases. Preventing patients from migrating into high cost tertiary care. The value proposition is not only to improve outcomes, but reduce the expense associated with healthcare utilization and medication consumption.
Diagram 3: Engagement is Reinforced with Self-Management Intervention
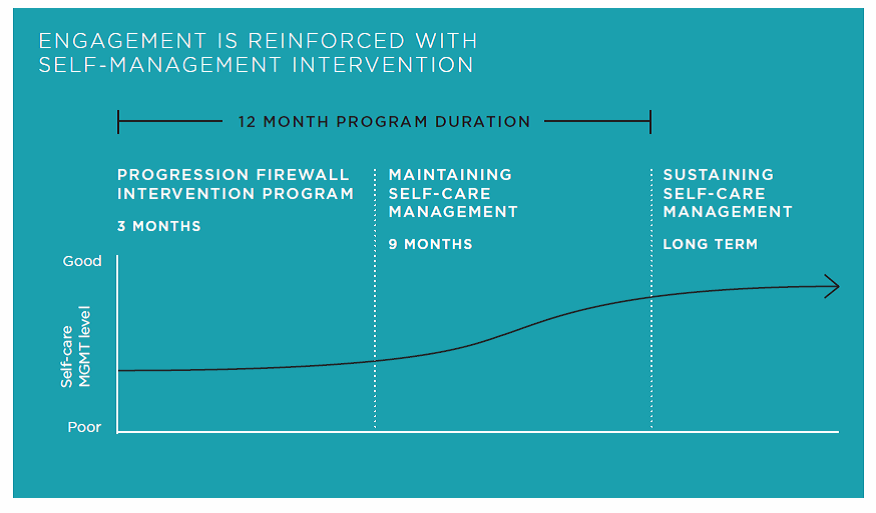
Unlike programs that are either digital or in-person, the OTS program was designed with engagement as the primary goal of the program. The professionals who developed the program recognized that the knowledge and techniques necessary for meaningful behavior change have existed for quite some time, but that the methodology had to be assembled around engagement. OTS is an example of a new category of interventions that is delivered outside the clinical space and shows great promise due to a focus on participation.
So which behavior change programs can most effectively address population groups that have been diagnosed with the onset of one or more chronic diseases, and what change measures are used to gauge success? Maybe we should rethink how program success is measured. It’s not outcomes only as that is just part of the story. Structure and processes impact outcomes.
Metrics-based management still reigns supreme for healthcare services. But to succeed, you need to know what to measure, how you will do that, and how to use that information to improve the program delivery. When in doubt, focus on improving participation. No matter what, if participation isn’t there, outcomes will not follow. Health system leaders know that value-based means quality-based population health participation. The transition to value is dependent on a health systems ability to deliver quality services that chronic disease population groups will use.
Diagram 4: Self-Management is Achieved following Quality Measures
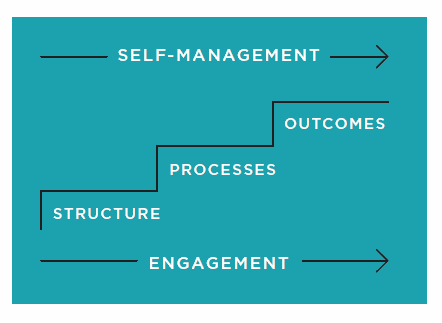
There is a wide variation in the structure and processes incorporated into behavior change program delivery to produce expected outcome results. Like clinical care, the healthcare industry needs to understand the metrics used by community care to ensure intensive lifestyle program delivery of chronic disease care.
OTS program participation is intensive (in-person and digital encounters), frequent (promoting consistent week-to-week core encounters for 12 weeks) during the initial intervention, and then during the nine months of maintenance. In-all, the program is delivered over 12 months to change and establish lifestyle habits related to the self-management of conditions. OTS is also designed to prevent premature drop-outs from the program. Participants develop the skills necessary to maintain long-term adherence and sustain new habits pertaining to diet, physical activity and underlying drivers of behavior.
To track MSHS employee population participation success, OTS collected the following measures:
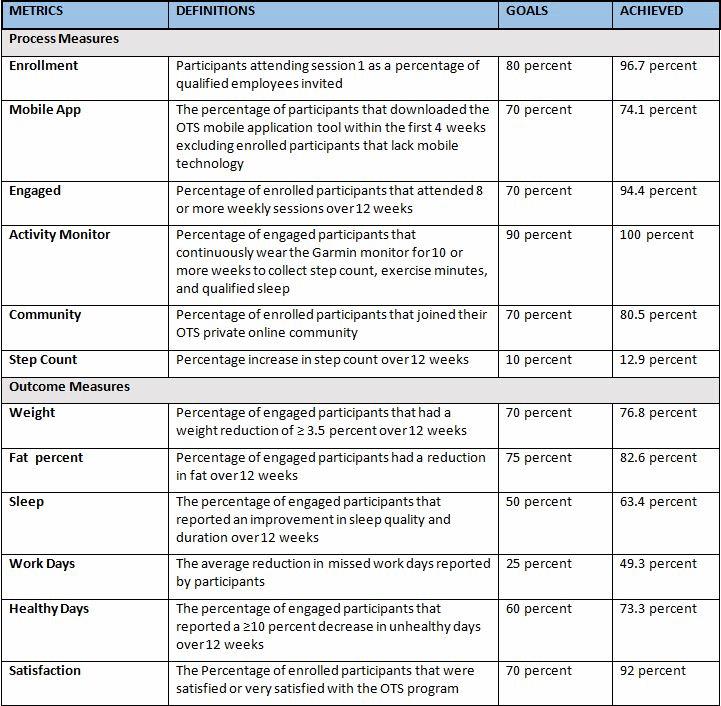
Participation is the most important indicator for change management and it is achieved by engagement. As value-based reimbursement and patient-centered care models strain to improve outcomes and reduce costs, the ability to evaluate behavior change programs by set standards is critical.
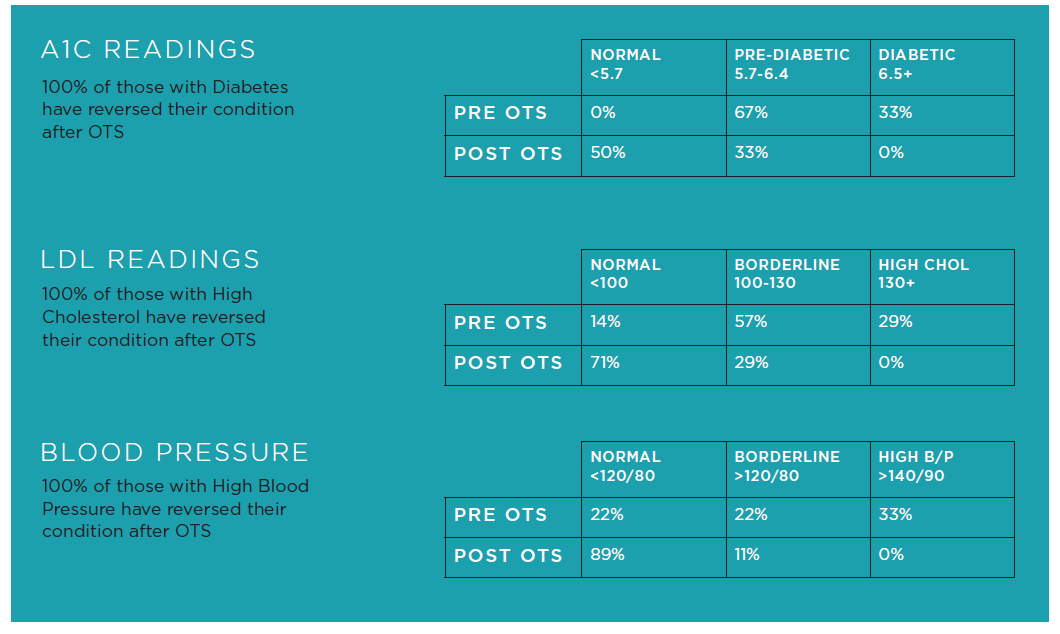
OTS Participants Showed Strong Long-Term Results After Completing Both The Three Month Intervention Period And The Nine Month Maintenance Period
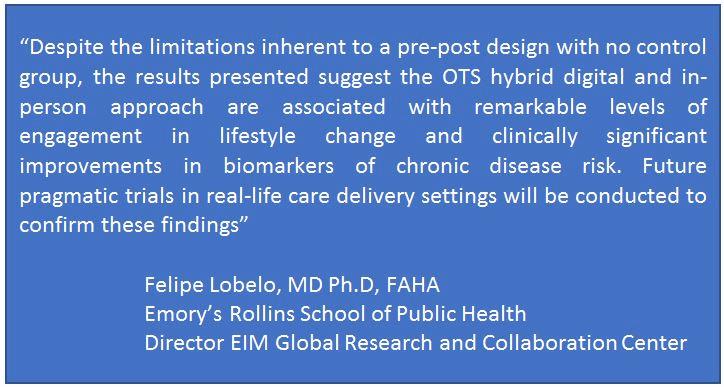
Participation is clearly the most important indicator for change management and it is achieved by engagement. As value-based reimbursement and patient-centered care models strain to improve outcomes and reduce costs, the ability to evaluate behavior change programs by set standards is critical.
The Future Of Behavior Change Programs
The dramatic increase in the prevalence, progressive nature and diagnosis of chronic disease is the main driver for the deployment of behavior change programs. The rise in disease-related comorbidities has also fueled a more aggressive approach to chronic disease management for the rising-risk. The main problem is that as chronic disease progresses, the patient loses the ability to self-manage their condition. The need for continuous behavior change engagement is necessary because most of the chronic disease care is in the hands of the patient. Therefore, the delivery of lifestyle intervention programs must have the intensity, frequency, and duration of engagement to change and maintain healthy lifestyles.
Health systems must examine their ability to scale behavior change program delivery for the rising-risk. Partnering with a community care organization that may have the quality measure evaluation criteria outlined above can reduce costs, increase quality of care, and improve health outcomes and patient satisfaction with community accessible programs.
Chronic diseases are the number one threat to America’s health because the rising-risk chronic disease population groups continue to move along the care continuum with higher rates of comorbidity driving higher costs of chronic disease care.
Saving Payers Money While Saving Patients From Unnecessary Procedures
For the last thirty years there have been plenty of ‘preventative wellness programs’ intended to keep people from developing chronic diseases. Beyond prevention there were limited options for patients who already had a chronic condition. Once an individual was diagnosed they were generally put on medication, told by their general practitioner to get some exercise and watch what they eat – and perhaps referred to a one-on-one meeting with a nutritionist. This solution is still the norm, and is not only costly for the payer, but ineffective for the patient. Off The Scale Health calls this the ‘care gap’ where patients are already sick enough to require medications and care, but not sick enough to warrant lap band surgery or other invasive operations. The Off The Scale BCI fills this care gap by providing a comprehensive program to reverse the disease. The BCI offers payers the option of reducing utilization and drug expenditures by improving the health of the patient, where before they simply spend money on medications and waited for the patient to get sick enough for surgery.
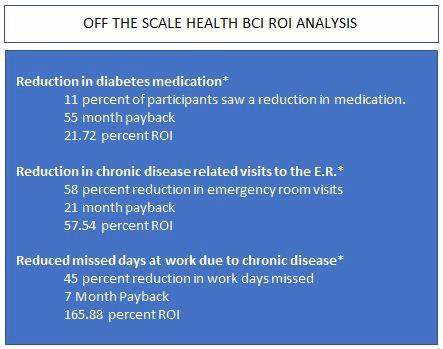
Directing patients to reverse their condition makes both clinical and financial sense. The reduction of utilization and drug spending is a measurable benefit. For employers the decrease in missed days is also compelling. The OTS BCI offers a very real return on investment as shown below.
About The Authors
Felipe Lobelo, MD PhD, FAHA
Emory’s Rollins School of Public Health
Director EIM Global Research and Collaboration Center
Phil Trotter, B.S.
Leads the Exercise is Medicine® (EIM) on-the-ground team to link Community Care with Clinical Care and the high value resources for community-based delivery of healthcare to payer, patient and underserved populations. Phil is a Community Care thought leader and Collaborative subject matter expert consulting with health system leadership and population health management executives and their teams.
Ashley John Heather, B.A.
Co-founder of Off The Scale® (OTS) a turnkey, chronic disease intervention platform.
F. Peter Brechter, B.A.
CEO of Off The Scale® (OTS) a turnkey, chronic disease intervention platform.
About Off The Scale
To learn more about OTS’s efficacy and results, email: outcomes@offthescale.com. Off The Scale was established in New York in 2014 by a team of healthcare, engagement, and technology executives. Their goal was to dramatically reduce the cost burden associated with global obesity and other chronic diseases. The Off The Scale Behavior Change Intervention
(BCI) is delivered through a multichannel platform, combining in person sessions, online community tools and mobile applications. The OTS platform delivers structured physical activity, nutritional education and lifestyle change action planning to maximize engagement, maintain long term participation and strong outcomes. This hybrid method makes it possible for substantial numbers of patients, employees and community residents to reverse their chronic condition. For more information visit www.offthescale.com.
Notes:
- CDC National Center for Chronic Disease Prevention and Health Promotion, At a Glance 2015
- American Hospital Association (AHA), Next Generation of Community Health 2016
- CDC The Four Domains of Chronic Disease Prevention, Working Toward Healthy People in Healthy Communities
- Public Health 2030, Chronic Disease Driver Forecasts
