How Tetris Can Transform Healthcare Operations

Serve 20 percent more patients at lower cost while reducing patient wait times by 30 percent.
By Jennifer Mensik, Chief Nursing Officer, LeanTaaS
Healthcare providers face an operational paradox — scarce resources are both overbooked and underutilized at the same time. The result? Long patient waiting times, frustrated patients, and unhappy nurses. With the growing demand for healthcare and not so promising supply of staff, there’s only one way to deal with it: Do more with less.
That’s easier said than done, isn’t it? But what if I told you that by doing just one thing right you can serve more patients, lower patient waiting times, and ensure your nurses eat lunch on time? It doesn’t involve adding more chairs or hiring more nurses — it’s as simple as playing Tetris right. That’s right, Tetris.
Let me explain.
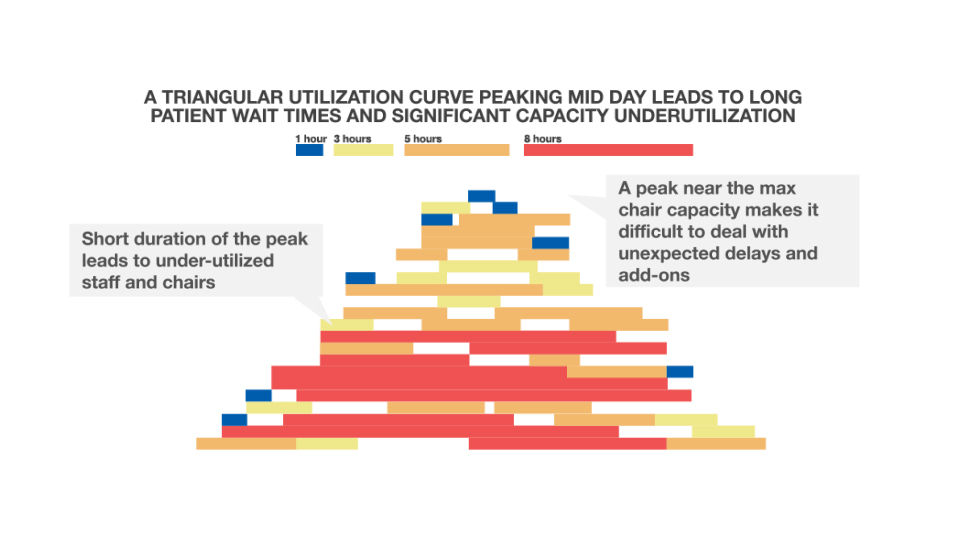
You are familiar with the typical daily pattern: The day starts slow, then things get really busy in the middle of the day, and then it slows down again. Just like Groundhog Day, it takes place in exactly the same way the next day and the next. It’s an interesting paradox — most people want to avoid the morning and evening rush hour but are stuck in the clinic or hospital because of the “provider rush hour.” At peak times, every minute of delay has a cascading effect resulting in chaos, frustration, and inefficiency:
- long patient wait times, unhappy patients, and overworked nurses
- underutilized resources in the mornings and evenings mean fewer patients seen than possible (and potential lost revenue)
- the sharp mid-day peak implies higher staffing levels leading to higher labor cost
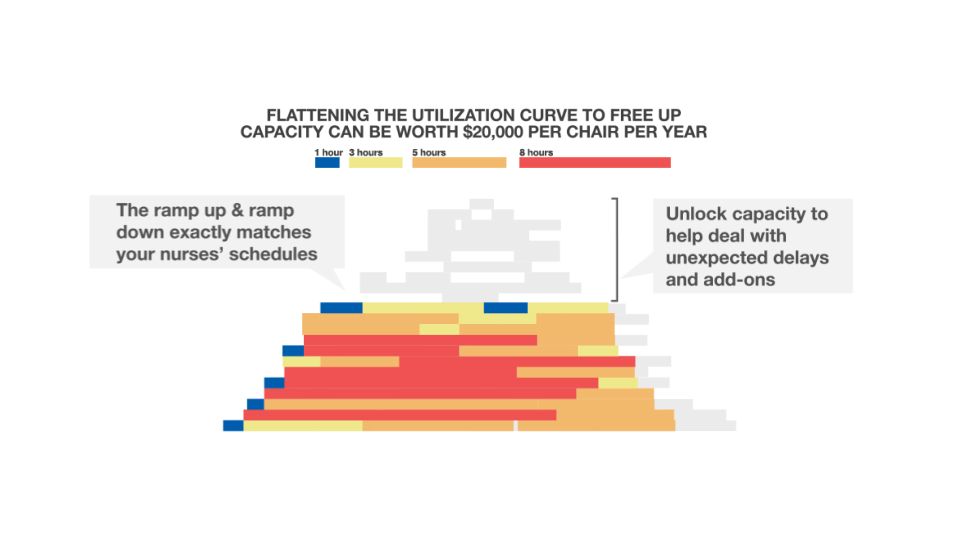
Over the last couple of years, we have worked with several healthcare centers on solving this problem. Solving it requires moving from a “peaky triangular profile” of utilization to a “level-loaded, flatter profile resembling a trapezoid” — not dissimilar from playing Tetris right. Getting to this flatter utilization profile could let you serve 20 percent more patients with reduced labor costs on a per-treatment basis.
It’s A Complex Problem
If you want to get to a flat utilization profile and see more patients every day, you need to steer patient appointments into a precise “fingerprint” pattern that is unique for each center for each hour of each day. This is not easy for several reasons. First, there are varying treatment times. Second, there are unexpected delays. Third, and most important, patients tend to prefer mid-day appointments. That leads to slow mornings, a mid-day rush and slow evenings. As a result, two bad things happen: severe overutilization around mid-day and severe underutilization the rest of the day. Underutilization results in lost revenue and reduced labor productivity. Overutilization results in long wait times for patients, higher labor costs and an acceleration in capital expenditures for adding chair capacity to the infusion center.
To illustrate the complexity, let’s take an example of a mid-sized infusion center that treats cancer patients. Infusion treatments generally tend to have fixed appointment lengths — you have 1 hour infusions, 2 hour infusions, 3 hour infusions, 9 hour infusions and so on. Many treatments tend to go longer than expected, but in general, they finish on time even if they start a bit late.
For the purposes of this example, let’s assume this infusion center has 30 chairs and sees approximately 70 patients a day. Infusion treatments come in different lengths (e.g., 1–2 hours, 3–4 hours and 5+ hours long), and the typical daily mix of patients for these three types are 35 patients, 25 patients and 10 patients, respectively.
The center schedules patients every 15 minutes starting at 8:00 a.m. with the last appointment offered at 5:30 p.m. So there are 39 possible starting time bands: 8:00 a.m., 8:15 a.m., 8:30 a.m., etc., ending at 5:30 p.m.
The center can accommodate three simultaneous patient starts due to the nursing workload of getting a patient situated, the IV connected and other prep. That makes a total of 39 *3 = 117 potential “appointment start slots.”
The number of ways in which the center can slot these 70 patients into the 117 slots available is 2.6 * 10^61 — a number with more than 60 zeroes!!
Tetris To The Rescue
The solution to this problem lies in understanding and employing the game of Tetris. If we can somehow “slot” all treatments in a day perfectly without any “gaps,” that would avoid the underutilization in the mornings and evenings and overutilization in the afternoons. Patients would arrive in a precise pattern and be flowed in a way similar to Tetris blocks falling precisely to the lowest level possible through the day. That means more unlocked capacity (and hence, more patients seen), higher revenue, less operational cost, and happy patients (and nurses)!
The first step in doing this is to mine the pattern of prior appointments in order to develop a realistic estimate of the volume and mix of appointment types for each day of the week going forward.
The second step is imposing the real operational constraints in the clinic (e.g., the hours of operation, doctor and nurse schedules, the number of chairs, various “rules” that depend on clinic schedules, as well as patient-centric policies such as treatments longer than four hours should be assigned to a bed and not a chair).
Finally, constraint-based optimization techniques can be applied to create the optimal “fingerprint pattern” of “slots,” which reflect the number of appointment starts of each duration for each hour of each day of the week.
In the case of the infusion center, that means a revised scheduling template that helps schedulers see how many one-hour duration, three-hour duration and five-hour duration slots can be made available at each possible start time (i.e., 7:00 a.m., 7:15 a.m., 7:30 a.m. and so on).
Doing this optimally results in moving the chair utilization graph from the “triangle” that peaks somewhere between 11:00 a.m. and 2:00 p.m. to a “trapezoid” that ramps up smoothly between 7:00 a.m. and 9:00 a.m., stays mostly flat from 9:00 a.m. until 4:00 p.m. and then ramps down smoothly from 4:00 p.m. onward.
Estimating The Potential Impact From “Playing Tetris Right”
To estimate the value, let us make a few simplifying assumptions:
- 30 infusion chairs (or beds), excluding those that are used for blood draws/port flushes
- $300 reimbursement per treatment (after drug expenses)
- 70 treatments on a typical, busy weekday
- 8 nurses on the floor in the middle of a typical, busy weekday
- 20 percent overtime pay on average
- $80,000 per year, per nurse (fully loaded annual cost per FTE)
- 10 percent growth in projected patient volumes per year
Level loading patient appointments can deliver improvements in the form of:
- 20 percent higher patient volumes (absorbing the next 1-2 years of growth without significantly increasing the staffing level or hours of operation)
- 30 percent reduction in patient wait times at the peak
- $546,000 increase in revenue (number of chairs * patients per chair per day * days of operation per week * 52 * percent additional treatments)
- $128,000 reduced labor costs from dramatically lowering overtime levels (by up to 50 percent) and from having a better FTE coverage due to the flatter load profile throughout the day
- The total impact of $674,000 total savings (works out to $22,466 per chair, per year)
Works For Most Appointments
This approach of data mining past appointments and applying constraints to perfectly “slot” patients evenly throughout the day works for most appointment types — doctor visits at a clinic, lab tests, equipment use such as MRI or CAT scan, surgery rooms, the ER and so on.
It’s fairly simple to bake in the last minute delays into the approach to achieve zero gaps even when things don’t go as planned. By “level loading” patients evenly throughout the day, the cascading effect of last minute delays at peak times (which is an operator’s worst case scenario) can be eliminated.
In any ecosystem, time adds complexity by design — there’s no way to avoid it. But by applying simple principles that are timeless, you can reverse the impact of complexity.
In this case, it’s as simple as the game of Tetris!
About The Author
Jennifer Mensik, PhD, RN, NEA-BC, FAAN, is the chief nursing officer at LeanTaaS. Jennifer holds a PhD in nursing, health systems and public administration from the University of Arizona College of Nursing. She has worked at St. Luke’s Health System in Idaho as the administrator for nursing and patient care and was the executive director of quality and patient safety for the UCLA Health System. She also worked at Banner Health as the system’s director of clinical practice and research. Jenifer is the author of multiple publications, including The Nurse’s Manager’s Guide to Innovative Staffing.
