Health Literacy: Improve Outcomes By Keeping Patients In The Know

By David Thompson, MD, CHC, FACEP, CEO and chief medical officer, Health Navigator
Imagine you’re a patient at the doctor’s office. You recently had surgery, and your doctor is explaining the aftercare instructions. But the words are complicated, the directions are complex, and you find yourself stuck. What would you do? This is a common problem that has significant consequences.
What Is Health Literacy?
According to the Institute of Medicine, health literacy is “the ability to obtain, process, and understand basic health information.” Many factors contribute to an individual’s health literacy including the person’s general literacy — the ability to read, write, and understand written text and numbers.
Other factors include a person’s amount of experience with the healthcare system, the type of information, culture, and the communication method.
Implications Of Limited Health Literacy
The National Center for Education Statistics performs a National Assessment of Adult Literacy (NAAL) every 10 years. The survey shows four levels of literacy: proficient, intermediate, basic, and below basic. In a world where healthcare is a must, limited literacy can pose challenges for providers in both traditional and telemedicine settings.
Although more than half of adult patients have adequate health literacy, many patients struggle to understand healthcare. Consider the following from the NAAL study:
- 26 percent of participants didn’t understand when their next appointment was scheduled
- 42 percent didn’t understand prescription instructions
- Up to 78 percent misinterpreted warnings on prescription labels
What does improving health literacy mean to patients and providers? For starters, improved disease management and reduced utilization. Consider this: Medicare enrollees with adequate literacy saw 4 percent fewer hospitalizations over three years than those with low literacy. And 33 percent of patients with adequate literacy had stable diabetes control versus 20 percent for patients with low literacy.
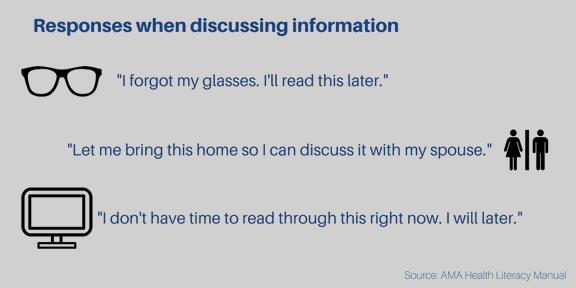
How To Tell If A Patient Has Limited Health Literacy
Based on the NAAL study, approximately 89 million American adults have limited literacy. Every day, physicians see patients who have trouble reading and understanding health information. Here are some clues that your patients may be struggling:
- missed appointments
- lack of follow through with laboratory and imaging tests
- lack of response to referrals
- noncompliance with medication regimens
Telehealth providers should also gather demographic data, as this can indicate risk among patients who are elderly, unemployed, do not have a high school diploma, have no insurance, don’t speak English (or have English as a second language), or have low to no income.
Regardless of whether you are face-to-face with a patient or providing care through telehealth technology, healthcare providers should ask all patients if they need help reading instructions or other written materials.
Enhancing Verbal Communication
Verbal communication decreases rates of stress, anxiety, and pain for patients. It can also improve patient satisfaction and increase compliance. These six steps can help improve verbal communication for physicians:
- slow down
- use plain language
- use visuals
- explain and repeat important concepts
- teach-back
- encourage questions
Enhancing Written Content
While verbal communication can help patients feel more comfortable, sometimes physicians need to use written content. When doing so, be sure to use patient-friendly language. In a telehealth encounter, use technology that provides plain language to patients. When writing, follow these guidelines:
- write at or below a sixth grade reading level
- use one- or two-syllable words and active voice
- write in short paragraphs
- use a large font (minimum 12 point)
- use bulleted lists instead of paragraphs
The Telehealth Solution
In addition to following health literacy principles, healthcare providers may benefit from using a telehealth platform that supports health literacy. Some platforms have the ability to convert plain language into coded medical terminology, which improves understanding for both patients and physicians.
Hospitals and healthcare systems can also use telehealth technology to train staff to use plain language communication, whether patient interactions are over the phone, through video or online.
The Provider’s Responsibility
Providers who recognize that improving health literacy is, in part, their duty can make healthcare more approachable and improve patient outcomes. Keep communication simple. Follow standard health literacy guidelines and use technology that delivers easy-to-use resources in patient-friendly language. Follow these steps to better communicate with patients, and ensure patients understand their care.
Make Your Office Patient-Friendly
To create a supportive environment for all patients consider the following:
- Scheduling appointments — Have a real person answering the phones. Collect only necessary information, and help patients prepare for their appointment.
- Office check-in procedures — Provide easy-to-read forms, and help patients fill them out.
- Referrals and supplementary tests — Provide directions to the referral and any information the patient may need. It may also help to license a telehealth platform that can provide printable summaries of patient encounters for other physicians.
- Patient instructions — Provide instructions and handouts in easy-to-read formats. Many diagnostic platforms can do this for you.
About The Author
David Thompson, MD, CHC, FACEP is CEO and chief medical officer at Health Navigator. A part-time faculty attending in the Northwestern Memorial Hospital Emergency Department, Dr. Thompson also serves as chief medical information officer for Schumacher Clinical Partners, and works as an author and partner with Self Care Decision, LLC and Schmitt-Thompson Clinical Content, LLC. In a collaboration with well-known pediatrician Dr. Barton Schmitt, Dr. Thompson has developed a comprehensive set of telephone triage protocols that are used in medical call centers and doctors’ offices in the United States and internationally. He is board-certified in both internal medicine and emergency medicine, having completed a dual residency at Northwestern Memorial Hospital at Northwestern University. Dr. Thompson is certified in healthcare compliance and is a Fellow in the American College of Emergency Physicians. He can be reached at david.thompson@healthnavigator.com.
