Enabling A Consumer eHealth Ecosystem With A Continuum of Connectivity

By Eric Abbott, director of product management and health facility technology, ExteNet Systems
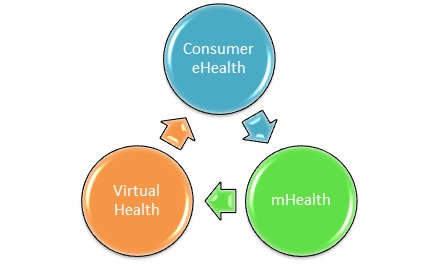
Consumer eHealth is empowering consumers through apps, social media, portals, medical devices, and other means to better manage and influence their health and wellness, access healthcare services, and improve workflows with their caregivers. In combination with mobile health (mHealth) modalities oriented around digital healthcare technologies, such as clinical diagnostics and electronic health record systems, and virtual health capabilities as exemplified by live, asynchronous clinical visits to a healthcare organization, this potent trifecta has the potential to fundamentally create a truly patient-centric ecosystem of health and wellness services.
Challenge
While the promise of consumer eHealth is unassailable, the execution of it underscored by recent studies demonstrates that many challenges remain. Notable examples include usability of applications (e.g., poor interfaces, complex tasks), privacy concerns (real or perceived), and the digital literacy of consumers, including terminology.
These challenges aside, real-time connectivity remains a juggernaut because patients and caregivers are mobile. In a very simplistic model, the consumer may be moving through a flux of different mobile technologies such as 4G and Wi-Fi. During these series of actions, any data sessions with digital healthcare systems tries to follow the user. But it’s not a seamless process and requires re-authentication and verification of the user in a best-case scenario. Summed up under the banner of interoperability, real-time performance of the app can suffer due to queuing/latency and different quality-of-service rules defined by different infrastructure management entities.
Compounding this is the meteoric growth in connected devices per patient, with projected estimates as high as 6.4 devices per patient per day. In a mobile setting, personal area network (PAN) devices such as wearables, internables, and consumables predominately use smartphones as an aggregation hub. In this scenario, these sensors, their controlling software, and even the governing app may ascribe different levels of service priority with different levels of security, presenting end-to-end encryption vulnerabilities. Now magnify this by the estimated 40,000-plus healthcare apps currently available, and the connectivity challenge becomes quite apparent.
Solution
Fortunately, the networking industry has developed sophisticated solutions that address many of these shortcomings in a transparent manner, which increases user confidence and trust in the solutions. This leads to repeatability and favorable behavioral changes, which drives adoption.
Consider the example of a patient with Type II diabetes – a treatable chronic medical condition facing millions of people. In this situation, an implantable diabetes insulin pump (internable) and a monitor (wearable) work together via APIs and a managed app on a smartphone to not only provide automatic alerts and notifications, but biometric data, long-term trend information, and even operating diagnostics. Similarly, in a clinical setting, use cases may include enterprise security around wireless point of care, role- and attribute-based services (presence, proximity, and location-based actions of Internet of Things, people, or machines), local content acceleration (e.g., rapid availability of large DICOM images for primary triage in emergency situations), and unified communications (secure text, voice, and imaging).
The creation of a seamless, heterogeneous healthcare “subnet” is a prime example of a real-time network capable of providing a continuum of connectivity to support healthcare and wellness services. Functionally, these technologies include cloud-based services, intelligent routing, virtualized parallel computing systems, disaggregated routing and authentication engines, and enterprise-oriented service archetypes with service aggregation and service edge modules. This managed framework may be linked together via service level agreements among an ecosystem of key workflow partners/vendors using key performance indicators and other means to ensure uniformity of service, security, privacy, and self-optimization.
In summary, the enabling network infrastructure to support a patient-centered healthcare system has come of age. It is neither one of wireless technologies nor one of networking equipment. Rather, it requires interoperable interworking of dedicated purpose systems with enabling technologies to provide intelligent services in a highly-scalable, available, and pervasive manner. The promise of a patient-centric ecosystem is here, but implementation requires a national consensus to build such a healthcare subnet. The question is this: who will rise to the challenge?
