Why Healthcare Needs Analytics: 12 Challenges Arising from COVID-19
By Andy Dé, Senior Director for Healthcare Solutions Strategy, Alteryx

From disrupted supply chains, and the inability to adequately protect patients and healthcare personnel, to massive shortages in capacity, drugs, devices, testing kits, and supplies – the novel coronavirus pandemic has created unprecedented challenges for healthcare providers and public health.
As we try to anticipate and avoid the second wave of COVID-19, there are still several important challenges confronting hospitals, health systems, and public health agencies; here, I have identified twelve. This list is by no means exhaustive, but an attempt to articulate some of the factors driving unprecedented strategic digital transformation in healthcare, both now and into the foreseeable future.
Contact Tracing and Rapid Response
Aggregating, transforming, and reporting on data about an outbreak like COVID-19 is now mission-critical, especially as restrictions lift in more states. Contact tracing is now necessary to trigger rapid response and contain the spread of the disease. We’ve seen some good evidence of success in countries that have instituted robust tracing measures, like Germany and South Korea.
Moreover, live dashboards like the one launched by The Center for Systems Science and Engineering at John Hopkins University at the onset of the pandemic, pull relevant data from the World Health Organization (WHO) and Centers for Disease Control (CDC) across the globe to show all confirmed and suspected cases of the coronavirus, along with recovered patients and deaths. The data is visualized through a real-time graphic information system (GIS).
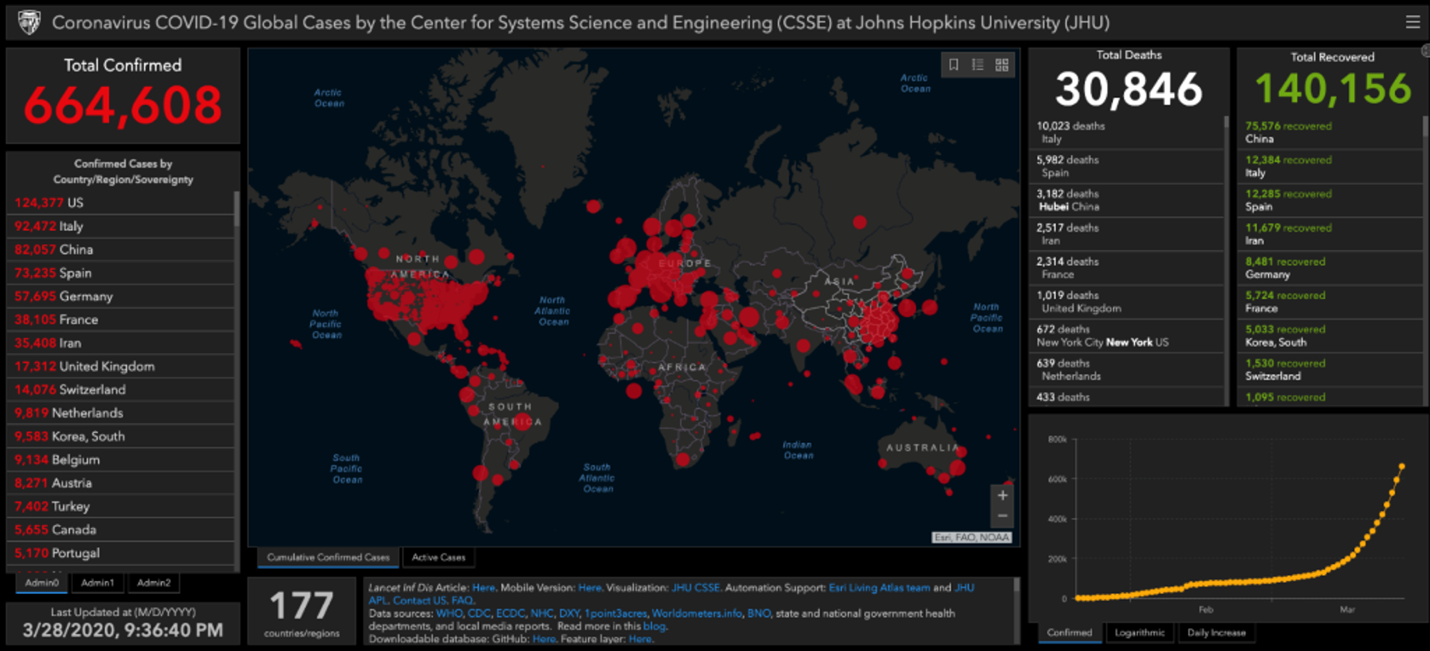
To avoid being caught off-guard again, healthcare providers and health systems will have to continually and proactively collaborate with the CDC, HHS, CMS – employing platforms like this – to plan for an unforeseen epidemic or pandemic outbreaks as a standard part of their strategic planning. Having solid data insights and acting on advanced intelligence is key to being one step ahead.
Securing Extra Capacity
Healthcare systems in large metropolitan areas have faced the prospect of not having the needed emergency, operation, and observation rooms to deal with the surge of patients infected with COVID-19. These providers must also embrace data analytics to help them strategically identify capacity in the event of another surge. Data-driven tools – like this solution from Vantage Data that maps and predicts ICU and hospitalization rates – can help them accomplish this.
Whether its monitoring and responding to these types of platforms in real-time, or using them to better understand the patterns of capacity in advance of an outbreak, using analytics could spell the difference between lives lost and saved when a surge strikes.
Recruiting Personnel from the Sidelines
Throughout the pandemic, we’ve heard reports lamenting the lack of doctors, nurses, and technicians to diagnose and treat patients quickly and effectively. One way of sourcing much-needed personnel back-up has been to hire retired clinicians and nurses to meet this need and alleviate the burden. Providers can use available databases and advanced analytics to locate retirees, surplus, and soon-to-graduate nurses, and physicians for sourcing purposes – both inside and outside of national borders.
Finding “At Risk” Patients
Healthcare providers have been challenged to segment non-COVID patients from those infected with the disease, and also to triage these patients based on risk (e.g. seniors over 65 and those with chronic conditions like cancer, COPD, diabetes, and cardiovascular disease).
By risk-stratifying patients based on demographic data, electronic medical records (EMRs), and socio-economic determinants of health, providers can proactively identify and prioritize the most vulnerable patients in a targeted way. To do this most accurately and assure optimal patient outcomes, data-driven stratification systems adopt descriptive and predictive analytics, machine learning, and natural language processing (NLP).
Triage via Telehealth/Telemedicine
We know that seniors and the immunocompromised are most vulnerable if infected, but these populations are often challenged in terms of their mobility and can struggle to access healthcare.
By leveraging existing tools like telehealth and telemedicine, healthcare professionals can now successfully triage, diagnose, and treat these patients remotely for non-acute conditions. Over the last few months, these systems have been well-utilized, lowering the risk of infection for these patients and their caregivers.
Advanced predictive analytics can be used to anticipate demand for these services and match patients with the right primary care physicians, specialists, nurses, and technicians.
Managing Burnout Among Healthcare Professionals
Not unexpectedly, medical professionals have become stressed and overworked while trying to meet the demands triggered by the surge in COVID-19. Too often, they have had to conduct their patient checks without the necessary personal protective equipment (PPE) to keep themselves safe.
Protecting healthcare professionals from risk, infection, and burnout is critical to alleviating the worst of the pandemic situation. Predictive analytics that helps manage PPE supply chains, staffing rotations, their physical and mental health and fatigue, and source additional personnel to help improve the working conditions.
Maximizing the Use of Provider Facilities
As referenced, many hospitals have been capacity constrained; particularly in terms of their ICUs, operating, and observation rooms. In earlier stages, many also suffered from a worrying lack of ventilators for their ICU beds.
In planning for any future surges, analytics will be key to demand-supply matching. Even within a facility, providers can use these tools to identify resources – like under-utilized beds that can be repurposed, or additional medical devices and diagnostic equipment – which could be critical for saving lives.
Forecasting Demand for Critical Drugs and Equipment
The COVID-19 pandemic has presented unprecedented and unforeseen challenges when it comes to the provision of medical staff, equipment, protective attire, drugs, and devices for hospitals. Leveraging demand data from this and previous epidemics (e.g. H1N1, Ebola, etc.) can help forecast demand for any future COVID-19 surge, as well as future similar health events.
By incorporating the demand data from this pandemic within Enterprise Resource Planning (ERP) or supply chain planning systems, and augmenting it with advanced predictive analysis, healthcare providers can significantly improve their levels of readiness.
Managing Supply Chain Disruption
Hospitals have been badly struggling with the process of securing new suppliers for testing kits and PPE while managing their existing supply chain. In addition, maverick (off-contract) buying is already a huge challenge that will likely have been exacerbated by the pandemic.
Hospitals now need to collaborate with entirely new suppliers, creating fresh supply chains while balancing this with their current supply chain to meet the needs of patients not afflicted by the outbreak. Self-service analytics can assist them in integrating data sources from ERP, EMR, and procurement to pinpoint the kind of buying that will ultimately save hospitals millions.
Managing Risk on 30-Day Re-Admissions
Many hospitals have experienced a surge due to the large numbers of patients infected with the coronavirus. This means that segmenting and stratifying patients who have been admitted based on risk will continue to be critical to saving lives.
Patients suffering from the harmful effects of the virus need to be isolated in the ICU with ventilators, sometimes for 20-30 days at a time. At the same time, physicians are treating and discharging patients with a lower risk profile to turn around hospital beds and free up capacity for new patients. There are sophisticated machine learning algorithms that healthcare providers could benefit from when managing this churn. These systems can be used to proactively identify the most vulnerable population of patients and prioritize them for advanced and more intensive care protocols in the ICUs with ventilators vs. younger patients less at risk.

Risk-based Patient Risk Stratification to match constrained capacity with the patients most at risk
Monitoring Hospital-Acquired Infections and Conditions
Hospital-acquired infections (HAIs) or hospital-acquired conditions (HACs) are now a greater risk given the large number of vulnerable patients passing through healthcare environments. The contraction of additional conditions could serve to worsen the plight of many patients.
Self-service descriptive and predictive analytics could be used by in-house staff to monitor metrics and KPIs (like Catheter-Associated Urinary Tract Infection (CAUTI) and central line-associated bloodstream infection (CLABSI) and laser-focus them to reduce their patient impact at this trying time.
Post-Discharge Monitoring
Many vulnerable patients will be susceptible to additional infections following discharge. These people should be proactively monitored for medication compliance, vital signs reporting, and follow-up appointments by care coordinators.
Here also, data analytics can be used to identify at-risk patients and proactively engage them using telehealth, remote patient monitoring, and videoconferencing. This kind of health surveillance will empower care coordinators to minimize 30-day re-admission risk while assuring superior patient outcomes.
In summary, there are several pressing challenges on our healthcare providers and professionals right now, and into the foreseeable future. Many of these could be helpfully managed with assistance from data analytics tools. What data insight gives healthcare staff is the ability to make better, more informed decisions. This couldn’t be more important than it is right now.
Disclaimer: The perspective and views expressed here are my own and do not represent those of my employers.
