Intervention Care For The 'Rising-Risk,' Before It's Too Late
The first white paper in this population health management (PHM) series, Chronic Disease is Healthcare’s Rising Risk, reported on the health and financial burden associated with chronic diseases, specifically the ‘rising-risk’ and ‘high-risk’ clinically stratified population groups. The second paper, A Health Behavior Change Framework for Population Health Management, set out a coordinated clinical-community structure for delivering chronic disease intervention care. This is the third white paper in this PHM series that will discuss the advantages of setting process and evaluation standards for methodology and community-digital engagement to achieve and sustain health behavior change for self-management.
Too late for what? Too late before the ‘rising-risk’ patients that have been diagnosed with one or more non-communicable chronic diseases migrating into ‘high-risk’, high cost care management.
There is a gap in care after patients have been diagnosed with one or more chronic diseases. The gap is associated with factors that, for the most part, are difficult to be effectively managed in every-day clinical healthcare delivery. This gap requires intervention care that addresses behavioral, social, environmental, and financial root causes that drive 80 percent of patient health outcomes.
Current chronic disease management typically focuses on one-to-one remote, light touch counseling sessions. Most health systems are not prepared to provide intervention care that is cohort program customized and peer group delivered combined with adequate intensity, frequency and duration digital engagement. High touch engagement approaches have demonstrated a greater likelihood of replacing unhealthy lifestyle behaviors.
A Change In PHM Focus
If there is one thing that most healthcare leaders can agree, it’s that population health management (PHM) programs can produce positive long-term health outcomes for the populations served and in so-doing be cost-effective for their systems and payers. This is supported by a growing body of evidence that PHM activities can curb the impact of chronic disease, lower unnecessary utilization of services, improve patient quality of life, and even help providers meet their value-based payment goals. This is particularly true for the stratified ‘rising-risk’ population groups where chronic disease can be impacted by intervention care behavior change.
Health systems PHM efforts most often focuses on managing ‘high-risk’ patients because they represent the highest care expense per person, and therefore the highest financial risk for health systems. However, while the ‘high-risk’ accounts for 35 percent of overall healthcare spending, the ‘rising-risk’ accounts for an even larger (51 percent) proportion. While improving care management for the ‘high-risk’ group is critical, it is also known that some of these patients with sky-high costs are often beyond the ability to intervene and impact outcomes. ‘Rising-risk’ patients on the other hand, can still benefit significantly from chronic disease management and evidence-based intensive intervention care programs. Because of strengthening secondary prevention, a reduction in healthcare utilization and cost for the ‘rising-risk’ and the ‘high-risk’ population groups are possible. This shift in focus should be a priority for health systems.
As ‘rising-risk’ patients move along the continuum of care and migrate closer to care management, health systems and payers increase their financial risk. This requires an all-out effort to slow, stop or even reverse disease progression. Clinical and community resources should be coordinated to build what was described as a firewall in the first white paper in this series. That firewall is meant to interrupt and if possible, block the flow of ‘rising-risk’ patients into the ‘high-risk’ patient care management population group. Until recently, the technology and knowledge did not exist to clearly stratify these groups and distribute chronic disease management resources accordingly to stop the flow into care management.
The development and availability of intervention care (secondary prevention) programs for the ‘rising-risk’ like care prevention (primary prevention) for the ‘low-risk’ are major steps for PHM to succeed. As an example, the Diabetes Prevention Program (DPP) is for ‘low-risk’ participants who are overweight, have family history of diabetes and/or have blood glucose levels higher than normal. Although these participants do not have high enough glucose levels for a diagnosis, they are at risk for developing frank diabetes in 5 to 10 years. The promotion of the DPP by government, non-profit and commercial entities has provided significant awareness and access as part of the wellness and healthy lifestyle movement in the U.S. However, once diagnosed with diabetes, intervention care programs take on greater sense of urgency with progression and comorbidities likely. Evidence and practice-based health behavior change methodologies with high-touch engagement strategies must then be implemented to meet the intervention care needs of a cohort in a standardized fashion.
Recognizing Intervention Care
The American College of Sports Medicine’s (ACSM) Exercise is Medicine (EIM) initiative has been at the forefront of advocating for chronic disease prevention and intervention, to establish physical activity as a standard in healthcare since 2007. EIM is credentialing qualified professionals that have a base knowledge of exercise prescriptions for chronic diseases, a working knowledge of changing health behaviors that contribute to the progression of chronic diseases, and understanding the important link between clinical care and community care.
As EIM credentials a national workforce of professionals to deliver intervention care programs, the EIM Global Research and Collaboration Center (GRCC), based at Emory University Rollins School of Public Health is working with ACSM to set frameworks and standards for effective intervention care programs to achieve self-management that leads to clinically significant outcomes. Health systems are looking for chronic disease management solutions that find, disrupt, and replace the root cause lifestyle habits of progression. To find real world answers, the GRCC is looking for practice-based evidence for intervention care programs that can be replicated with comparable results as a standard of care for diagnosed chronic diseases while in parallel advancing the evidence-base on effectiveness and cost-effectiveness of standardizing these clinical-community linkages.
Health Systems Filling Intervention Care Gaps
Before the rapid adoption of value-based care, health systems considered evidence to be the result of clinical trials and post-approval studies that took years and sometimes decades to complete. However, the advent of electronic health records, patient-generated data via wearables and a host of data collection and analytical tools has changed the playing field. With the digital revolution providing the ability to track process and outcome data, health systems can more readily identify the factors in people’s lives that influence the effectiveness of treatments and therapeutic programs. They can see the extent to which extenuating circumstances, such as gaps in treatment, influence outcomes. Armed with this information, they can contemplate new strategies to fill those gaps for patients.
Mount Sinai Health System (MSHS) is an example of a system that has positioned itself ahead of the chronic disease intervention curve by delivering intervention care to their employees stratified into chronic disease population groups. Organizations like MSHS are opting to bolster their approaches to combating chronic disease progression by adding turnkey intervention care solutions like the Off The Scale® (OTS) intervention to their existing programs. They are executing on strategies to limit their exposure to ‘high-risk’ population groups by reducing ‘rising-risk’ migration. “My grandmother used to say that prevention is better than a cure,” said Sudipto Srivastava, Senior Director, eHealth, Mount Sinai Health System. “Interventions including the use of digital tools paired with behavior changes before health conditions become unmanageable can be extremely powerful. Organizations that can leverage digital health solutions like Off the Scale, fine tune the algorithms based on evidence, and incorporating these solutions into enterprise workflows can make a significant improvement in patient outcomes and costs.”
Pioneering Intervention Care
Health systems are moving forward to find intervention care solutions. The EIM-GRCC is working to establish intervention care process and outcome standards by evaluating practice-based evidence from EIM, OTS, the Medical Fitness Association (MFA) care protocols, and other intervention care program providers. These standards offer the guidance that health systems need to effectively implement intervention care programs, and there is a lot to consider. Program delivery is a natural process starting with digital or face-to-face (community) as options. However combined community and digital can potentially the “best of both worlds” for increased engagement to modify unhealthy lifestyle behaviors. In any case, an iterative process is likely to measure multiple community and digital touch points to drive the level of engagement required for an evidence-based change methodology to succeed. A methodology that identifies unhealthy behaviors, replaces them with healthier choices, and practices these new behaviors until new routines become sustainable (self-managed) requires high engagement. Engagement is critical to the process of replacing the root causes of chronic diseases to improve the short and long term return in the form of improved outcomes.
The advantages of group versus individual sessions go beyond the obvious economic efficiencies. In the group environment participants give and receive support by reinforcing positive behaviors and discouraging unhealthy ones within the group. The classic example of this positive behavior change through support is Alcoholics Anonymous. The process of peer group support is particularly challenging for cohorts that include individuals that may vary from those just diagnosed with a chronic disease, to early progression to late progression. Will cohort stage of progression also impact levels of engagement? It may be that the latter stages of progression and therefore those patients closer to migrating into ‘high-risk’ care management will need increased levels of engagement duration, frequency and intensity to achieve chronic disease self-management.
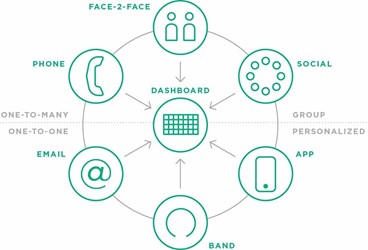
Best practices in behavioral change science center on understanding patients and helping them identify personal motivators for change.12 Replicable methodologies that identify, change and help replace personal motivators encourage participants to make long-term lifestyle changes. As the EIM-GRCC process and outcome standards are established, the criteria for evaluating programs based on achieving self-management will be the objective. Each element of engagement process must be managed at levels that achieve change momentum and avoid engagement relapse. Some insight can be gained from the OTS approach at Mount Sinai Health System where a 360-engagement model (see below) for methodology delivery and tracking touch points illustrates a replicable program for cohort to cohort.
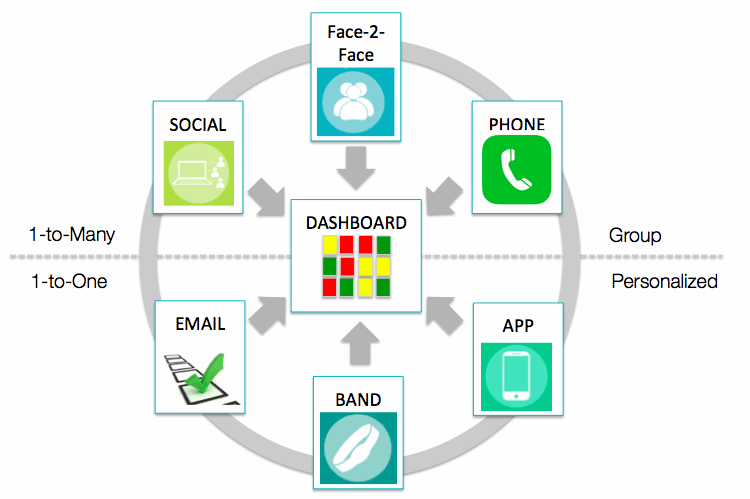
Source: Provided by Off the Scale (OTS), 2016.
The task ahead for EIM-GRCC is to evaluate OTS and all other intervention care programs with practice-based evidence to track small and cumulative successes that create the confidence patients with chronic disease need when attempting health behavior change. No doubt patients with higher risk scores may need to receive extra attention, including more frequent follow-up along with more social and community support. It is hypothesized that each patient will reach their particular “threshold of change” when the engagement frequency and intensity achieves the right “dose” to drive behavior change while accounting for preferences and barriers. The EIM-GRCC will be looking for data that validates the “sweet spot” for this threshold. Is it achieved after 4-6 weeks of the program initiation? If so will 8 to 6 weeks allow sufficient time to reinforce that change? This field needs as much “real-world” data that intervention care program providers can contribute to refine and validate the EIM-GRCC and ACSM to establish a comprehensive set of process and outcome standards and produce the type data health systems need to advance their PHM and value-based care models.
As the evaluation of intervention care programs evolve, these standards can guide the combination of engagement duration, frequency and intensity that creates an effective balance to achieve optimal results from a program methodology perspective. During the intervention and maintenance periods, monitoring self-care management progress and relapses will be analyzed to determine if better overall health on the group and individual basis is achieved. When deployed in close coordination with a health system’s PHM team, including access to healthcare utilization and costs, the EIM-GRCC can assist health systems objectively assess the community care program impact in achieving all dimensions of the Quadruple AIM: improving the patient and provider experience, lowering per capita costs, and raising the overall level of health for populations.
Intervention Care Evaluation
Clinical patient engagement to change lifestyles is typically a high cost approach. The EIM-GRCC will be evaluating the delivery of intervention care delivered as a group-based program in lower-cost community settings as part of the Quadruple AIM value-based care solution. The EIM-GRCC is taking the lead in the evaluating ‘community’ data alongside clinical and claims data to measure intervention care impact on patients with chronic diseases. As an independent evaluation and analytics academic hub, the EIM-GRCC will be collecting specific community data that tracks engagement during the intervention process relying on sources from wearables, mobile apps, surveys, professional feedback, and patient self-reports. This data provides the basis for intervention care program process and outcomes evaluation that culminates in establishing the level of self-management achieved.
It’s Not Too Late, In Fact It’s Just Beginning
Clearly it is not too late to focus on disease management for the ‘rising-risk’ population groups before they migrate to ‘high-risk’ care management. On the contrary, now is the time for health systems to use their PHM resources to stratify ‘rising-risk’ population groups from their employees or value-based payer populations for intervention care. Intervention care programs are becoming available to help slow, stop and reverse the progression of chronic diseases by implementing structured, high-engagement behavior change. In doing so, PHM can reduce the population groups that are responsible for the largest portion of patient care expense. Advancing intervention care programs can create the rare instance of a win-win for patients, providers, and the communities served.
About The Authors
Felipe Lobelo, MD Ph.D., is an associate professor of Global Health at Emory’s Rollins School of Public Health and directs the EIM Global Research and Collaboration Center (EIM-GRCC). The EIM-GRCC is the academic hub in charge of leading the evaluation of the EIM initiative, in collaboration with partnering healthcare systems, community organizations, and fitness and technology companies.
Phil Trotter, B.S., leads the Exercise is Medicine® (EIM) on-the-ground team to link Community Care with Clinical Care and the necessary resources for community-based delivery of healthcare to payer, patient and underserved populations. Phil is a Community Care thought leader and Collaborative subject matter expert consulting with health system leadership and population health management executives and their teams.
Ashley John Heather, B.A., co-founder of Off The Scale ® a turnkey, chronic disease intervention platform.
Adrian Hutber, Ph.D., was appointed Vice President of Exercise is Medicine® (EIM) at the American College of Sports Medicine (ACSM) in 2008, after serving as the vice president of a fitness corporation and as the Director of the Distance Education Division of the world’s largest physical activity publisher, Human Kinetics. EIM is the multi organizational, multi-national initiative co-founded by the American Medical Association and ACSM – and subsequently managed by ACSM.
