Fighting For Provider Revenue

By Ken Congdon
Healthcare reform, reimbursement cuts, sequestration, and RAC and Meaningful Use audits are new financial challenges cutting into provider revenue. How can you cope?
It’s a tough time to be a healthcare provider. The industry is going through a colossal shift that, while much needed, is causing a fair amount of pain for health systems, hospitals, physician practices, and other organizations that deliver patient care. Many of the systemwide changes occurring in healthcare are hitting providers where it hurts most — the balance sheet.
 For example, healthcare reform aims to fundamentally change the way providers are reimbursed — moving from the traditional fee-for-service system to a pay-forperformance model where groups of healthcare providers are jointly accountable and appropriately reimbursed for the quality of care they provide patients. As if restructuring your entire financial operation in line with this new model weren’t enough, Medicare has imposed several (and often substantial) reimbursement cuts to various providers over the past few years. Internal medicine, radiology, and oncology were among the specialties most affected by the cuts. Moreover, sequestration levied an additional 2% in Medicare cuts across the board starting in April of this year.
For example, healthcare reform aims to fundamentally change the way providers are reimbursed — moving from the traditional fee-for-service system to a pay-forperformance model where groups of healthcare providers are jointly accountable and appropriately reimbursed for the quality of care they provide patients. As if restructuring your entire financial operation in line with this new model weren’t enough, Medicare has imposed several (and often substantial) reimbursement cuts to various providers over the past few years. Internal medicine, radiology, and oncology were among the specialties most affected by the cuts. Moreover, sequestration levied an additional 2% in Medicare cuts across the board starting in April of this year.
The federal government isn't only cutting back on how much it pays you. It’s going after monies it has already disbursed. RAC audits are asking providers to prove they were reimbursed appropriately for services provided or give back the funds initially awarded. Likewise, Meaningful Use audits require further proof of successful attestation, or incentive dollars are reclaimed by CMS.
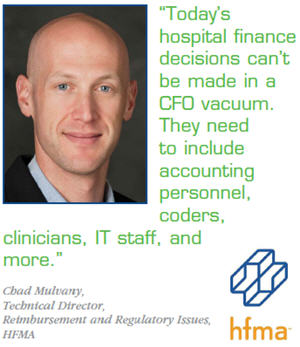
“There are a ton of new financial challenges being thrown at providers all at once,” says Chad Mulvany, technical director of reimbursement and regulatory issues at HFMA (Healthcare Financial Management Association). “Not only are Medicare payments being cut, but commercial sector reimbursement is also being stifled. To complicate matters, healthcare providers don’t have the money to hire the staff typically necessary to do all the things they are being required to do — whether it’s appeal to an RAC audit, transition to ICD-10, or implement EHR technology in a meaningful way. Failure to address these areas could ultimately lead to more lost revenue in the form of penalties.”
All the federal hoops providers are being forced to jump through have prompted many to cut their ties with Medicare and Medicaid. This is changing the patient dynamic, not only for providers that no longer accept government payers, but also for those who still do.
 LEAN MANAGEMENT ESSENTIAL TO RESHAPING FINANCIAL PROCESSES
LEAN MANAGEMENT ESSENTIAL TO RESHAPING FINANCIAL PROCESSES
Providers will continue to face downward revenue pressure regardless of whether they continue to work with government payers or not. Commercial insurance companies are also being forced to re-examine their reimbursement rates to stabilize profits and provide competitive premiums. However, success in this new healthcare world is possible. Providers just need to be willing to rethink their financial processes from the ground up.
“Hospitals need to apply lean management concepts to their processes in order to weather the new demands of the industry,” says Mulvany. “They need to question all of their existing processes and ask how these processes can be more efficient.”
There are two predominant lean schools of thought — Six Sigma and Kaizen. Both philosophies are focused on improving processes by eliminating waste and reducing defects, but each takes a slightly different approach to achieving this outcome. For example, Six Sigma incorporates more statistical analysis than Kaizen, focusing on eliminating defects so that the final product is as close to perfection as possible. Kaizen, on the other hand, looks to improve all aspects of business by standardizing processes and eliminating waste. Kaizen also strives to include every employee — from C-level executives to entry-level workers — in the process improvement initiative. According to Mulvany, this “community” approach to lean is very important in healthcare.
“It would be unwise to ignore culture during this transitional period in healthcare,” says Mulvany. “The most successful organizations are typically those that manage change the best. The key to effective change management is ensuring all stakeholders impacted by a process are involved in modifying that process. Health providers need to map out all the folks affected by their financial processes and ensure they have a seat at the table. Today’s hospital finance decisions can’t be made in a CFO vacuum. They need to include accounting personnel, coders, clinicians, IT staff, and more.”
Once key financial processes are modified and made as efficient as possible by applying lean concepts, then providers can begin to evaluate technologies to automate aspects of these processes and make them even more efficient. However, Mulvany suggests you bring lean thinking into the technology realm as well.
“Before going out and spending thousands of dollars on a new technology solution, healthcare providers should start by taking a closer look at the technology they already have in place,” he says. “Over the past few years in particular, many healthcare organizations have invested in a number of health IT tools that are currently being underemployed. In many instances, systems you’ve already invested in can be applied to address new demands.”
FOCUS ON PERFECTING FRONT END COLLECTION
Of all the financial pressures currently facing healthcare providers, it seems like the biggest concern among many is effectively addressing the expected rise in patient financial responsibility. “With healthcare reform and the emergence of health insurance exchanges, we are going to see an increase in policies that behave like high-deductible plans,” says Mulvany. “Many employers are going to be forced to offer these plans in an effort to cut costs, while many healthy self-insured individuals will opt for a high-deductible insurance option. This trend is going to make front end collection processes much more important for healthcare providers.”
According to Carrie Moneymaker, operations manager at Medical Management Professionals (MMP), a physician billing and practice management service provider, this trend toward high-deductible health insurance is already occurring. Moneymaker advises providers to be proactive in establishing a policy and technology infrastructure to determine eligibility and accept and manage patient payments.
 “Healthcare providers need to have a system in place that tells them what patients will owe up front,” says Moneymaker. “Then, providers need to decide whether they are going to collect that entire amount before service is rendered, or if they will collect a portion of it and establish a payment plan for the remainder.”
“Healthcare providers need to have a system in place that tells them what patients will owe up front,” says Moneymaker. “Then, providers need to decide whether they are going to collect that entire amount before service is rendered, or if they will collect a portion of it and establish a payment plan for the remainder.”
Orthopaedic Specialists of the Carolinas (OSC), for example, has adopted a strategy to collect patient payments at the time of service. “We use Navicure Eligibility to determine if patients are covered for specific services before performing them,” says Regina Hayes, Business Office Manager at OSC. “We then determine what their financial responsibility will be for that procedure — whether it’s an MRI or surgery — and collect those amounts prior to the appointment. We will work with individuals under special circumstances to establish a payment plan, but for the most part, we collect payment up front. The healthcare industry is changing, and we’re trying to help patients understand that part of this change means that medical costs need to be considered as part of their daily finances — just like groceries or rent.”
Of course, proper education is essential to ensuring that patients understand their financial responsibilities and adhere to your terms. Both Moneymaker and Hayes agree that the provider should play a significant role in this education process rather than leaving it up to the payer or the patients themselves.
“Providers need to prepare their patients ahead of time for what they may owe because many folks don’t have a clear idea of what their insurance plan actually covers,” says Moneymaker. “If a provider informs the patient up front about what their responsibility will be, the patient won’t be shocked when they receive the bill and will be more apt to pay it in a reasonable fashion. This also eliminates a bunch of the administrative time wasted by answering phone calls from patients with questions about their bill.”
Providers can further ensure that they receive timely payments from patients by providing convenient billing options. Healthcare has been stuck in a paper world for far too long, and paper bills, EOBs, and checks have only served to needlessly delay communications between providers and patients while adding to the administrative costs healthcare organizations endure. It’s high time providers at large embrace the online billing and payment options that have been mainstays in retail and finance for years now.
Many patients will still opt for paper correspondence, but those who take advantage of online billing and payment options can have a significant impact on your bottom line. For example, OSC has offered online billing and payment via its website for more than three years and saw 15% to 20% of its patient population use this service in the first three months of availability. OSC has recently extended its online capabilities by integrating its website and online patient billing system with its NextGen EHR patient portal. Now, patients can not only pay their bills and view their EOBs online, they can also gain access to their electronic health records.
“Consumers have become so accustomed to accessing information online,” says Hayes. “It’s become an expectation of doing business. Healthcare providers need to offer this capability not only for patient convenience, but also to streamline their own processes. Every transaction that is completed online is posted to our billing system and the money is deposited right in the bank. There’s no paper handling or manual posting, which saves time and money.”
Increased patient financial responsibility will undoubtedly change healthcare provider collection processes and priorities, but according to Mulvany this may actually be a positive shift. “If healthcare reform rolls out as anticipated, providers will have to collect a higher volume of small-dollar claims from patients with high-deductible plans, but there should be fewer catastrophic balances,” he says. “At the end of the day, it’s an improved situation to be in.”
