ACOs: Healthcare's Future, Or An Inevitable Failure?

By John Oncea, Editor
Follow John on Twitter: @buck25
Accountable Care Organizations are being referred to by some as the business model of the future, while others aren’t nearly as optimistic
The term Accountable Care Organization has been around since 2006 and, in 2009, became part of the healthcare industry landscape when it was included in the Patient Protection and Affordable Care Act.
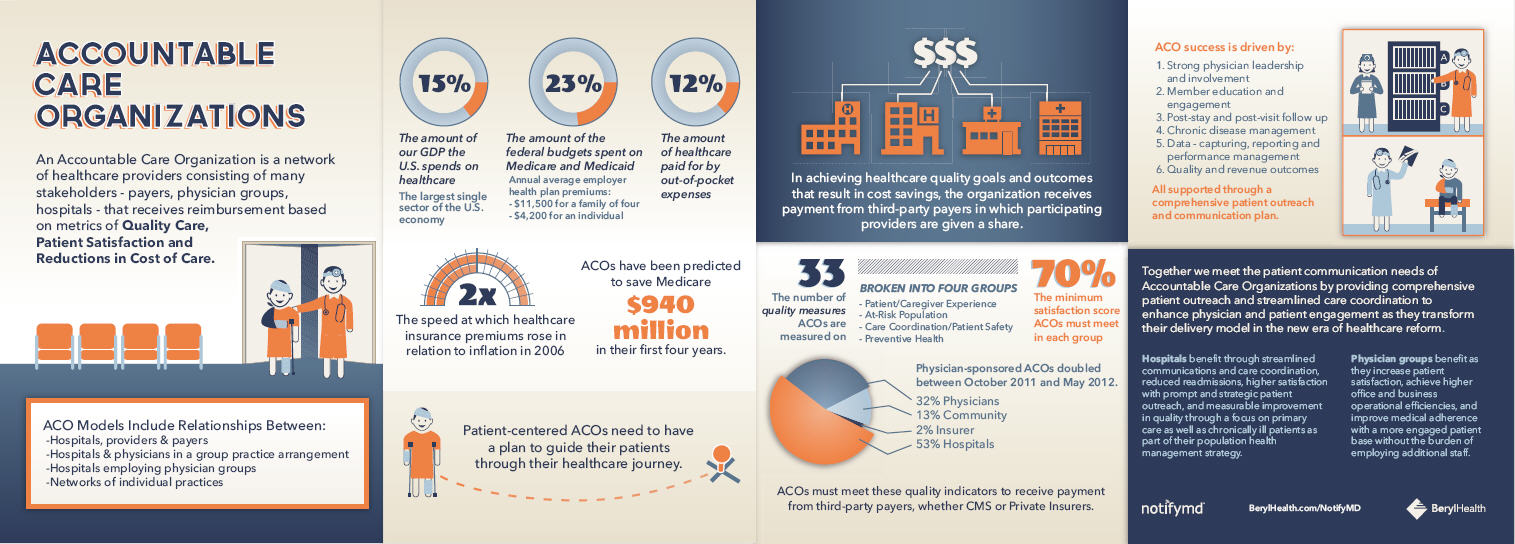
BerylHealth created this infographic which provides a wealth of ACO-related information from the amount of the U.S. GDP spent on healthcare (15%) to the number of quality measures ACOs are measured on (33).
Click here or on the image to view a larger version
Becker’s Hospital Review, while noting, “There is no perfect formula for ACO success that will work for all organizations,” lays out three ACO readiness strategies “that, if developed properly, are proven to contribute greatly to the success of an ACO.” Becker’s refers readers to this Aegis Health Group thought paper which provided more details on the three strategies.
The Aegis approach is just one of many. The New York Times singles out Kaiser Permanente as a model people often have in mind when talking about the future of healthcare. The Times notes Kaiser “combines a nonprofit insurance plan with its own hospitals and clinics, (and) is the kind of holistic health system that President Obama’s healthcare law encourages.”
HealthLeaders Media points to another ACO success, referring to MissionPoint Health Partners as “moving the needle forward.” MissionPoint surpassed its goal of 15,000 first-year members by more than 35,000 and cut the medical costs each year for its 15,000 original members by 12%, an “indication that this ACO model is not only viable, but could be a lesson in how-to for other hospitals and systems considering plans to set up these new models of care.”
Not everyone sees a bright future for ACOs, however. The Wall Street Journal published an opinion column calling ACOs “updated versions of HMOs” that are “based on flawed assumptions about doctor and patient behavior.” The column concludes that ACOs “over the long haul may ease the path to slightly lower reimbursements or redistribute physician compensation among specialties. But what ACOs most assuredly will not do is deliver the disruptive innovation that the U.S. health-care system urgently needs.”
HealthCare IT News echoes those sentiments quoting Jim Hansen, vice president of the Accountable Delivery System Institute for Lumeris, as saying “Without systemic changes – the desire to change the way healthcare is delivered – an ACO is most likely doomed to failure.”